By Hai Fang, Peking University
China achieves near-universal coverage through the provision of publicly funded basic medical insurance. The urban employed are required to enroll in an employment-based program, which is funded primarily via employer and employee payroll taxes. Other residents can voluntarily enroll in Urban-Rural Resident Basic Medical Insurance, financed primarily by central and local governments through individual premium subsidies. Local health commissions organize public and private health care organizations to deliver services. The basic medical insurance plans cover primary, specialty, hospital, and mental health care, as well as prescription drugs and traditional Chinese medicine. Deductibles, copayments, and reimbursement ceilings apply. There is no annual cap on out-of-pocket spending. Complementary private health insurance helps cover cost-sharing and coverage gaps.
Sections
How does universal health coverage work?
China largely achieved universal insurance coverage in 2011 through three public insurance programs1:
- Urban Employee Basic Medical Insurance, mandatory for urban residents with formal jobs, was launched in 1998.
- The voluntary Newly Cooperative Medical Scheme was offered to rural residents in 2003.
- The voluntary Urban Resident Basic Medical Insurance was launched in 2007 to cover urban residents without formal jobs, including children, the elderly, and the self-employed.
In 2016, China’s central government, the State Council, announced that it would merge the Newly Cooperative Medical Scheme and Urban Resident Basic Medical Insurance to expand the risk pool and reduce administrative costs.2 This consolidation is still underway. The combined public insurance program is now called Urban-Rural Resident Basic Medical Insurance.
Because China has a huge population, insurance coverage was increased gradually. In 2011, approximately 95 percent of the Chinese population was covered under one of the three medical insurances. Insurance coverage is not required in China.
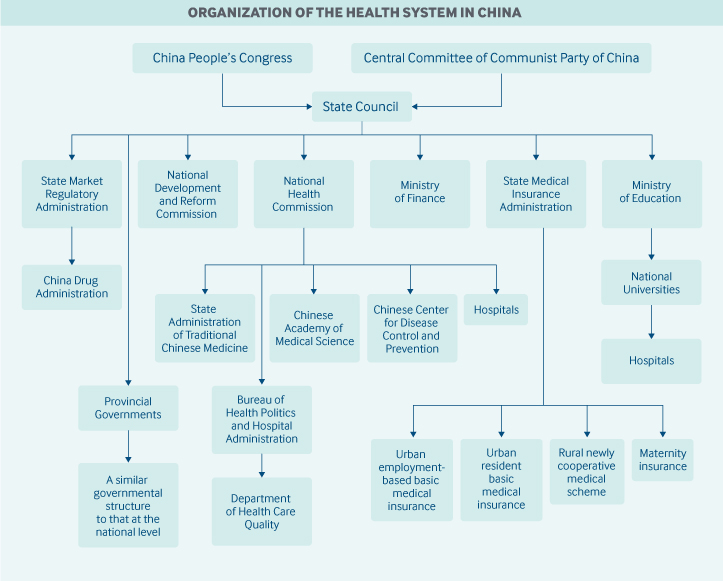
Role of government: China’s central government has overall responsibility for national health legislation, policy, and administration. It is guided by the principle that every citizen is entitled to receive basic health care services. Local governments — provinces, prefectures, cities, counties, and towns — are responsible for organizing and providing these services.
Both national and local health agencies and authorities have comprehensive responsibilities for health quality and safety, cost control, provider fee schedules, health information technology, clinical guidelines, and health equity.
In March 2018, the State Council reorganized the central government’s health care structure. The responsibilities of various agencies include the following:
- The National Health Commission is the main national health agency. The commission formulates national health policies; coordinates and advances medical and health care reform; and supervises and administers public health, medical care, health emergency response, and family planning services. The State Administration of Traditional Chinese Medicine is affiliated with the agency.
- The State Medical Insurance Administration oversees the basic medical insurance programs, catastrophic medical insurance, a maternity insurance program, the pricing of pharmaceutical products and health services, and a medical financial assistance program.
- The National People’s Congress is responsible for health legislation. However, major health policies and reforms may be initiated by the State Council and the Central Committee of the Communist Party, and these are also regarded as law.
- The National Development and Reform Commission oversees health infrastructure plans and competition among health care providers.
- The Ministry of Finance provides funding for government health subsidies, health insurance contributions, and health system infrastructure.
- The newly created State Market Regulatory Administration includes the China Drug Administration, which is responsible for drug approvals and licenses.
- The China Center for Disease Control and Prevention, although not a government agency, is administrated by the National Health Commission.
- The Chinese Academy of Medical Science, under the National Health Commission, is the national center for health research.
Local governments (of prefectures, counties, and towns) may have their own commissions, bureaus, or health departments. Centers for disease control and prevention also exist in local areas and are likewise administered by local commissions, bureaus, or health departments. At the national level, the China Center for Disease Control and Prevention provides only technical support to the local centers.
Role of public health insurance: In 2018, China spent approximately 6.6 percent of GDP on health care, which amounts to CNY 5,912 billion (USD 1,665 billion).3 Twenty-eight percent was financed by the central and local governments, 44 percent was financed by publicly funded health insurance, private health insurance, or social health donations, and 28 percent was paid out-of-pocket.4
Urban Employee Basic Medical Insurance is financed mainly from employee and employer payroll taxes, with minimal government funding. Participation is mandatory for workers in urban areas. In 2018, 316.8 million had employee-based insurance.5 The base of the employee payroll tax contribution is capped at 300 percent of the average local salary; individual payroll above this level is not taxed. In most provinces, individual tax rates are about 2 percent. Tax rates for employers vary by province. The base for employer contributions is the sum of employees’ payrolls. Workers’ nonemployed family members are not covered.
Urban-Rural Resident Basic Medical Insurance covers rural residents and urban, self-employed individuals, children, students, elderly adults, and others. The insurance is voluntary at the household level. In 2018, 897.4 million were covered under the two insurance schemes (the rural plan and the urban nonemployed plan) that make up this program.
Urban-Rural Resident Basic Medical Insurance is financed through annual fixed premiums. Individual premium contributions are minimal, and government subsidies for insurance premiums make up the majority of insurer revenues. In regions where the economy is less developed, the central government provides a much larger share of subsidies than provincial and prefectural governments. In more-developed provinces, most subsidies are locally provided (mainly by provincial governments).
The few permanent foreign residents are entitled to the same coverage benefits as citizens. Undocumented immigrants and visitors are not covered by publicly financed health insurance.
Role of private health insurance: Purchased primarily by higher-income individuals and by employers for their workers, private insurance can be used to cover deductibles, copayments, and other cost-sharing, as well as to provide coverage for expensive services not paid for by public insurance.
No statistics are available on the percentage of the population with private coverage. Private health insurance is provided mainly by for-profit commercial insurance companies.
The total value of private health insurance premiums grew by 28.9 percent per year between 2010 and 2015.6 In 2015, private health insurance premiums accounted for 5.9 percent of total health expenditures.7 The Chinese government is encouraging development of the private insurance market, and some foreign insurance companies have recently entered the market.
Services covered: The benefit package is often defined by the local governments. Publicly financed basic medical insurance typically covers:
- inpatient hospital care (selected provinces and cities)
- primary and specialist care
- prescription drugs
- mental health care
- physical therapy
- emergency care
- traditional Chinese medicine.
A few dental services (such as tooth extraction, but not cleaning) and optometry services are covered, but most are paid out-of-pocket. Home care and hospice care are often not included either. Durable medical equipment, such as wheelchairs and hearing aids, is often not covered.
Preventive services, such as immunization and disease screening, are included in a separate public-health benefit package funded by the central and local governments; every resident is entitled to these without copayments or deductibles. Coverage is person-specific; there are no family or household benefit arrangements.
Maternity care is also covered by a separate insurance program; it is currently being merged into the basic medical insurance plan.
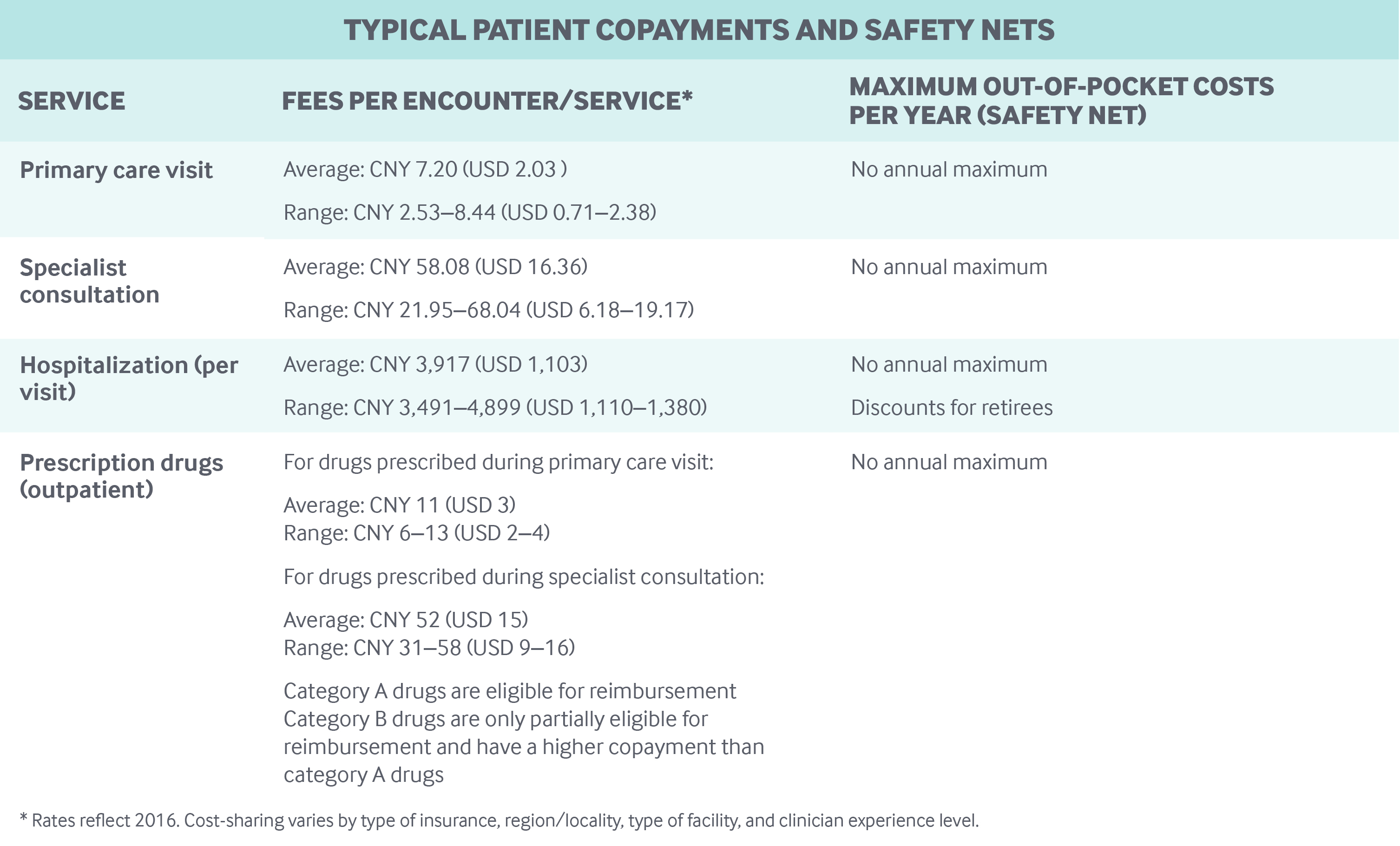
Cost-sharing and out-of-pocket spending: Inpatient and outpatient care, including prescription drugs, are subject to different deductibles, copayments, and reimbursement ceilings depending on the insurance plan, region, type of hospital (community, secondary, or tertiary), and other factors:
- Copayments for outpatient physician visits are often small (CNY 5–10, or USD 2–3), although physicians with professor titles have much higher copayments.
- Prescription drug copayments vary; they were about 50 percent to 80 percent of the cost of the drug in Beijing in 2018, depending on the hospital type.
- Copayments for inpatient admissions are much higher than for outpatient services.
There are no annual caps on out-of-pocket spending. In 2018, out-of-pocket spending per capita was CNY 1,186 (USD 262)—representing about 28 percent of total health expenditures.8 A fairly high percentage of out-of-pocket spending is for prescription drugs.
The public insurance programs only reimburse patients up to a certain ceiling, above which residents must cover all out-of-pocket costs. Reimbursement ceilings are significantly lower for outpatient care than for inpatient care. For example, in 2018, the outpatient care ceiling was CNY 3,000 (USD 845) for Beijing residents under Urban-Rural Resident Basic Medical Insurance. In comparison, the ceiling for inpatient care was CNY 200,000 (USD 56,338). Annual deductibles have to be met before reimbursements, and different annual deductibles may apply for outpatient and inpatient care.
Preventive services, such as cancer screenings and flu vaccinations, are covered by a separate public health program. Children and the elderly have no copayments for these services, but other residents have to pay 100 percent of these services out-of-pocket.
People can use out-of-network health services (even across provinces), but these have higher copayments.
Safety nets: For individuals who are not able to afford individual premiums for publicly financed health insurance or cannot cover out-of-pocket spending, a medical financial assistance program, funded by local governments and social donations, serves as a safety net in both urban and rural areas.
The medical financial assistance program prioritizes catastrophic care expenses, with some coverage of emergency department costs and other expenses. Funds are used mainly to pay for individual deductibles, copayments, and medical spending exceeding annual benefit caps, as well as individual premiums for publicly financed health insurance. In 2018, 76.7 million people (approximately 5.5% of the population) received such assistance for health insurance enrollment, and 53.6 million people (3.8% of the population) received funds for direct health expenses.9
How is the delivery system organized and how are providers paid?
Physician education and workforce: The number of physicians is not regulated at the national level, and the government is trying to encourage more people to complete medical school. All the medical schools are public. Tuition varies by region, ranging from CNY 5,000 (USD 1,408) to CNY 10,000 (USD 2,816) per year. Tuition is heavily subsidized by the government.
To ensure a supply of medical providers in rural or remote areas, China waives tuition and lowers entrance qualifications for some medical students. Medical students who attend these education programs must work in rural or remote areas for at least six years after graduation.
Primary care: Primary care is delivered primarily by:
- Village doctors and community health workers in rural clinics
- General practitioners (GPs) or family doctors in rural township and urban community hospitals
- Medical professionals (doctors and nurses) in secondary and tertiary hospitals.
In 2018, there were 506,003 public primary care facilities and 437,636 private village clinics. Village doctors, who are not licensed GPs, can work only in village clinics. In 2018, there were 907,098 village doctors and health workers. Village clinics in rural areas receive technical support from township hospitals.
Patients are encouraged to seek care in village clinics, township hospitals, or community hospitals because cost-sharing is lower at these care sites than at secondary or tertiary hospitals. However, residents can choose to see a GP in an upper-level hospital. Signing up with a GP in advance is not required, and referrals are generally not necessary to see outpatient specialists. There are few localities that use GPs as gatekeepers.
In 2018, China had 308,740 licensed and assistant GPs, representing 8.6 percent of all licensed physicians and assistant physicians.10 Unlike village doctors and health workers in the village clinics, GPs rarely work in solo or group practices; most are employed by hospitals and work with nurses and nonphysician clinicians, who are also hospital employees.
Nurses and nonphysician clinicians are sometimes employed as care managers or coordinators to assist GPs in treating patients with chronic illnesses or complex needs. Care coordination is generally not incentivized well, although it is always encouraged by health authorities.
Fee schedules for primary care in government-funded health institutions are regulated by local health authorities and the Bureaus of Commodity Prices. Primary care doctors in public hospitals and clinics cannot bill above the fee schedule. To encourage nongovernmental investment in health care, China began allowing nonpublic clinics and hospitals to charge above the fee schedule in 2014.11
Village doctors and health workers in village clinics earn income through reimbursements for clinical services and public health services like immunizations and chronic disease screening; government subsidies are also available. Incomes vary substantially by region. GPs at hospitals receive a base salary along with activity-based payments, such as patient registration fees. With fee-for-service still the dominant payment mechanism for hospitals (see below), hospital-based physicians have strong financial incentives to induce demand. It is estimated that wages constitute only one-quarter of physician incomes; the rest is thought to be derived from practice activities. No official income statistics are reported for doctors.
In 2018, 42 percent of outpatient expenses and 28 percent of inpatient expenses, on average, were for prescription drugs provided to patients in hospitals.12
Outpatient specialist care: Outpatient specialists are employed by and usually work in hospitals. Most specialists practice in only one hospital, although practicing in multiple settings is being introduced and encouraged in China. Specialists receive compensation in the form of a base salary plus activity-based payments, with fee schedules set by the local health authorities and Bureaus of Commodity Prices.
Patients have a choice of specialist through their hospital. Outpatient specialists are paid on a fee-for-service basis through the hospitals in which they work, and specialist doctors in the public hospitals cannot bill above the fee schedule.
Administrative mechanisms for direct patient payments to providers: Patients pay deductibles and copayments to hospitals for primary care and specialty physician office visits, and for hospital admissions at the point of service. Hospitals bill insurers directly for the remaining covered payment at the same time through electronic billing systems.
After-hours care: Because village doctors and health workers often live in the same community as patients, they voluntarily provide some after-hours care when needed. In addition, rural township hospitals and urban secondary and tertiary hospitals have emergency departments (EDs) where both primary care doctors and specialists are available, minimizing the need for walk-in, after-hours care centers. In EDs, nurse triage is not required and there are few other restrictions, so people can simply walk in and register for care at any time. ED use is not substantially more expensive than usual care for patients.
Information on patients’ emergency visits is not routinely sent to their primary care doctors. Patients can call 120 or 999 for emergency ambulance services at any time.
Hospitals: Hospitals can be public or private, nonprofit or for-profit. Most township hospitals and community hospitals are public, but both public and private secondary and tertiary hospitals exist in urban areas.
Rural township hospitals and urban community hospitals are often regarded as primary care facilities, more like village clinics than actual hospitals.
In 2018, there were approximately 12,000 public hospitals and 21,000 private hospitals (excluding township hospitals and community hospitals), of which about 20,500 were nonprofit and 12,600 were for-profit.13
The National Health Commission directly owns some hospitals in Beijing, and national universities (directly administrated by the Ministry of Education) also own affiliated hospitals. Local government health agencies in each province may have a similar structure and often own provincial hospitals.
Hospitals are paid through a combination of out-of-pocket payments, health insurance compensation, and, in the case of public hospitals, government subsidies. These subsidies represented 8.5 percent of total revenue in 2018.14
Although fee-for-service is the dominant form of provider payment, diagnosis-related group (DRG) payments, capitation, and global budgets are becoming more popular for inpatient care in selected areas. Pay-for-performance is rare. Local health authorities set fee schedules, and doctors’ salaries and other payments are included in hospital reimbursements. There are no special allowances for the adoption of new technologies.
Mental health care: Diagnosis, treatment, and rehabilitation of mental health conditions is provided in special psychiatric hospitals and in the psychology departments of tertiary hospitals. Patients with mild illnesses are often treated at home or in the community clinics; only severely mentally ill patients are treated in psychiatric hospitals. Mental health care is not integrated with primary care.
Outpatient and inpatient mental health services are covered by both public health insurance programs (Urban Employee Basic Medical Insurance and Urban-Rural Resident Basic Medical Insurance). In 2018, there were 42 million mental health patient visits to special psychiatric hospitals; on average, one psychiatrist treated 4.7 patients per day.15
Long-term care and social supports: Long-term care and social supports are not part of China’s public health insurance.
In accordance with Chinese tradition, long-term care is provided mainly by family members at home. There are very few formal long-term care providers, although private providers (some of them international entities) are entering the market, with services aimed at middle-class and wealthy families. Family caregivers are not entitled to financial support or tax benefits, and long-term care insurance is virtually nonexistent; expenses for care in the few existing long-term care facilities are paid almost entirely out-of-pocket.
The government has designated 15 cities as pilot sites for long-term care insurance, with the aim of developing a formal national policy framework by 2020. Local governments often provide some subsidies to long-term care facilities.
On average, conditions in long-term care facilities are poor, and there are long waiting lists for enrollment in high-end facilities. Formal long-term care facilities usually provide housekeeping, meals, and basic services like transportation, but very few health services. Some, however, may coordinate health care with local township or community hospitals.
Governments encourage the integration of long-term care with other health care services, particularly those funded by private investment. There were 3.8 million beds for aged and disabled people in 2016.16
Some hospice care is available, but it is normally not covered by health insurance.17
What are the major strategies to ensure quality of care?
The Department of Health Care Quality, which is within the Bureau of Health Politics and Hospital Administration and is overseen by the National Health Commission, is responsible at the national level for the quality of care. The National Health Service Survey for patients and providers is conducted every five years (the latest was in 2018), and a report is published after each survey highlighting data on selected quality indicators. Management programs for chronic diseases are included in the Essential Public Health Equalization Program and are free to every Chinese citizen.
To be accredited, hospitals must obtain a license from the local health authority. Physicians get their practice licenses through hospitals; licenses are subject to renewal. Local health authorities are responsible for physician recertification and revalidation and for hospital accreditation to ensure competency. Several national rankings of hospitals are published by third parties, although there are no financial incentives for hospitals to meet quality targets.18 No public information about individual doctors, nursing homes, or home care agencies is made available.
Following release of the “Temporary Directing Principles of Clinical Pathway Management” by the former Ministry of Health in 2009, clinical pathways are now regulated nationally and used similarly to clinical guidelines in Western countries. Previously, pathways were created at the hospital, rather than the national, level.
What is being done to reduce disparities?
There are still severe disparities in the accessibility and quality of health care, although China has made significant improvements in this regard in the past decade. Income-related disparities in health care access were especially serious before the reform of the health insurance system more than 10 years ago, as most people did not have any coverage at all. Health coverage through publicly financed insurance is now nearly universal, and there are safety nets for the poor (see above). As a result, income-related disparities have been reduced substantially. However, there is no oversight agency to monitor or report on health disparities and there are no targeted programs to reduce disparities for specific groups.
Remaining disparities in access are due mainly to variation in insurance benefit packages that are determined locally, urban and rural factors, and income inequality. Urban Employee Basic Medical Insurance offers lower cost-sharing than Urban-Rural Resident Basic Medical Insurance. Central and local government subsidies to Urban-Rural Resident Basic Medical Insurance have increased in recent years.
Most good hospitals (particularly tertiary hospitals) with better-qualified health professionals are in urban areas. Village doctors are often undertrained. To help bridge the urban–rural health care gap, the central government and local governments sponsor training for rural doctors in urban hospitals and require new medical graduates to work as residents in rural health facilities. Nevertheless, the China Health Statistical Yearbook shows that substantial disparities remain.
What is being done to promote delivery system integration and care coordination?
Medical alliances of regional hospital groups (often including one tertiary hospital and several secondary hospitals) and primary care facilities provide primary care for patients. The aims are to reduce unnecessary visits to tertiary hospitals, cut health care costs, and improve efficiency. At the same time, patients with serious health problems can be referred to tertiary hospitals easily and moved back to primary care facilities after their condition improves. The hospitals within a medical alliance share a common electronic health record (EHR) system, and lab results, radiology images, and diagnoses are easily available within the alliance. It is hoped that this type of care coordination will meet the demand for chronic disease care, improve health care quality, and contain rising costs, but it is rarely employed efficiently.
There are three main medical alliance models.19 Hospitals in the Zhenjiang model have only one owner (usually the local bureau of health). Those in the Wuhan model do not belong to the same owner, but administration and finances are all handled by one tertiary hospital. Hospitals in the Shanghai model share management and technical skills only; ownership and financial responsibility are separate. The Shanghai model is dominant in China.
What is the status of electronic health records?
Nearly every health care provider has set up its own EHR system. Within hospitals, EHRs are also linked to the health insurance systems for payment of claims, with unique patient identifiers (insurance ID or citizenship ID). However, EHR systems vary significantly by hospital and are usually not integrated or interoperable. Patients often must bring with them a printed health record if they want to see doctors in different hospitals. Even if hospitals are owned by the same local bureau of health or affiliated with the same universities, different EHR systems may be used.
Patients generally do not use EHR systems for accessing information, scheduling appointments, sending secure messages, refilling prescriptions, or accessing doctors’ notes. There is no national strategy for establishing standardized EHR systems; however, some regions are in the preliminary stages of planning to establish regional EHRs.
How are costs contained?
Health expenditures have risen significantly in recent decades because of health insurance reform, an aging population, economic development, and health technology advances. Health expenditures increased from CNY 584 (USD 164) per capita in 2004 to CNY 4,237 (USD 1,194) in 2018.20
Provider payment reform is one key cost-containment strategy. Prior to the 2009 introduction of DRGs, global budgets, and capitation, fee-for-service was the main payment mechanism, and consumer- and physician-induced demand increased costs significantly. Global budgets have been used in many regions; these are relatively easy for authorities to implement.
As noted above, the government also encourages the use of community and township hospitals over the more expensive care provided in tertiary hospitals. Hospitals compete on quality, level of technology, and copayment rates.
In township, community, and county hospitals, a campaign of “zero markups” for prescription drugs was introduced in 2013 to contain rising drug costs. This program was extended to secondary and tertiary hospitals in many regions.
In addition, the National Development and Reform Commission and National Health Commission place stringent supply constraints on new hospital buildings and hospital beds, and they also control the purchase of high-tech equipment, such as MRI scanners.
What major innovations and reforms have recently been introduced?
In March 2018, the 13th National People’s Congress unveiled a plan for restructuring its biggest cabinet (the State Council) in order to improve efficiency and public services (see above).

