By Karsten Vrangbæk, University of Copenhagen
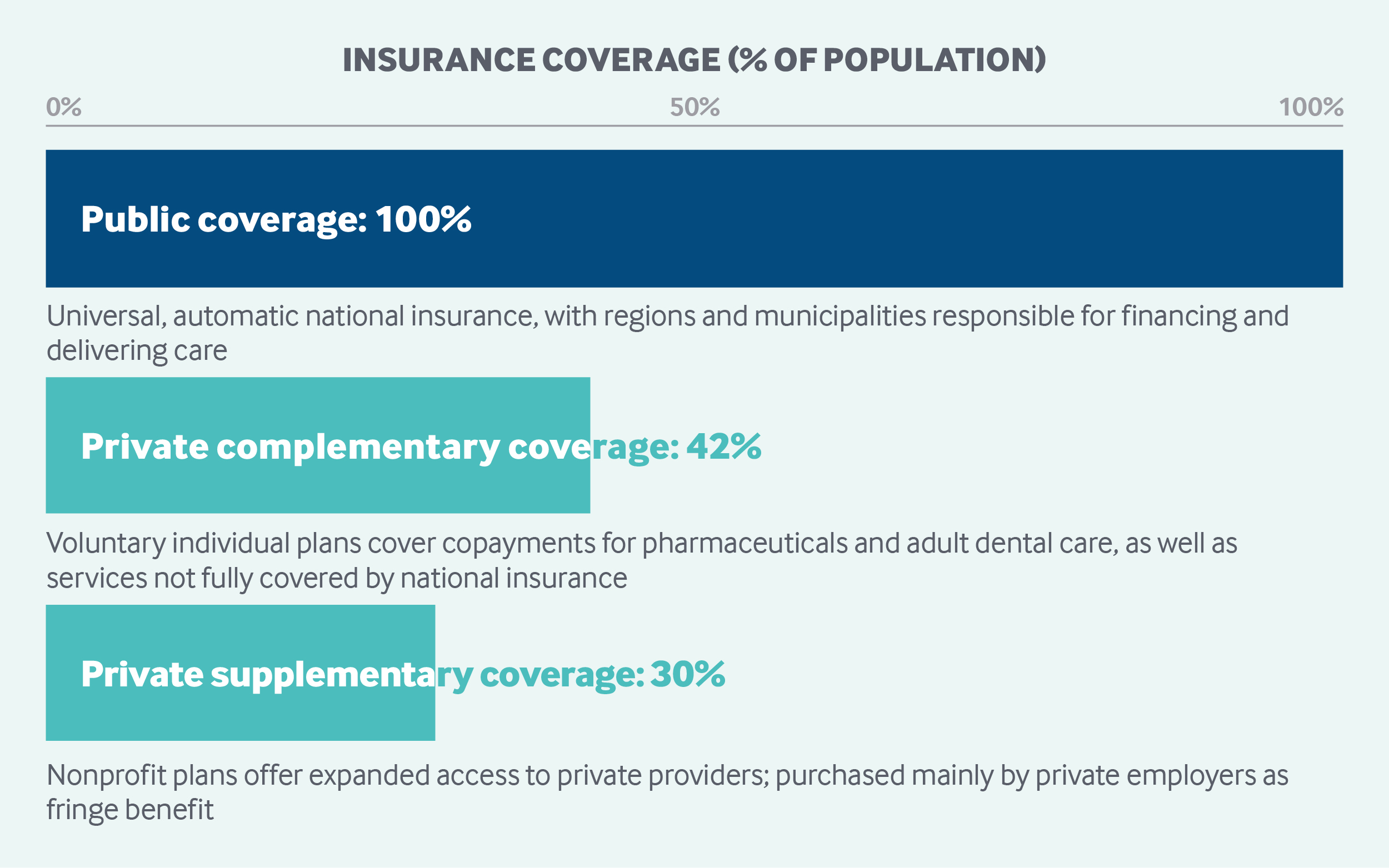
In Denmark’s universal, decentralized health system, the national government provides block grants from tax revenues to the regions and municipalities, which deliver health services. All residents are entitled to publicly financed care, including largely free primary, specialist, hospital, mental health, preventive, and long-term care services. Residents may purchase voluntary complementary insurance to cover copayments for outpatient drugs, dental care, and other services. Supplemental insurance, provided mainly by private employers, offers expanded access to private providers. Cost-sharing limits for adults and for children create a safety net.
Sections
How does universal health coverage work?
All registered Danish residents are automatically enrolled in publicly financed health care, which is largely free at the point of use. Registered immigrants and asylum-seekers are also covered, while undocumented immigrants have access to acute-care services through a voluntary, privately funded initiative supported by the Danish Medical Association, the Danish Red Cross, and the Danish Refugee Council.
Danes can choose from two public insurance options. Practically all Danes (98%) choose Group 1 coverage, under which general practitioners (GPs) act as gatekeepers and patients need a referral to see specialists, except for a few specialties. The remaining 2 percent of Danes choose Group 2 coverage, which allows access to specialists without a referral, although copayments apply. Under both insurance options, access to hospitals requires a referral.
Universal access to health care underlies Denmark’s Health Law, which sets out the government’s obligation to promote population health and prevent and treat illness, suffering, and functional limitations; to ensure high-quality care and easy and equal access; and to promote service integration, choice, transparency, access to information, and short waiting times.
Universal coverage developed gradually, starting in the latter part of the 1800s with nongovernmental insurance, known as sickness funds, covering primary care and user charges for hospital care. In 1973, the current universal public coverage system was founded through legislative reform.
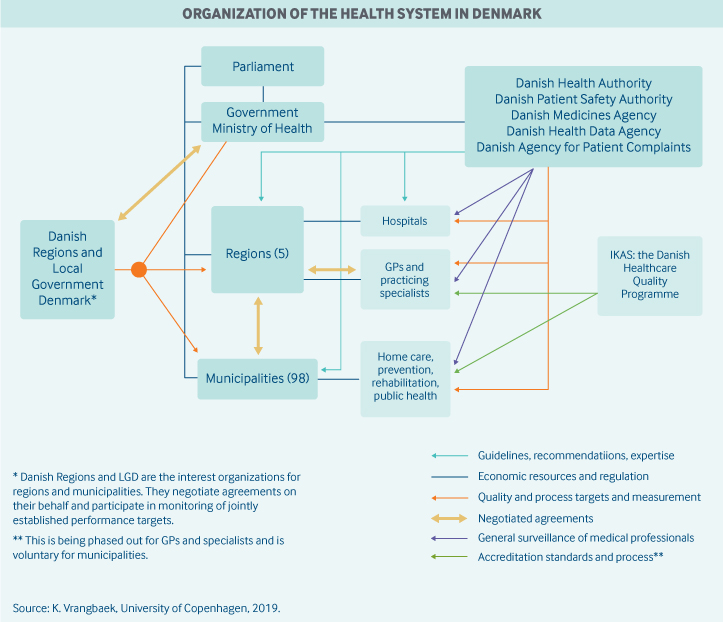
Role of government: The national government sets the regulatory framework for health services and is in charge of general planning, monitoring care quality, and licensing health care professionals. The national government also collects taxes and allocates funding to regions and municipalities based on sociodemographic criteria and activity.
The state does not have a direct role in the delivery of health care services. Five regions governed by democratically elected councils are responsible for the planning and delivery of specialized health care services and play a role in specialized social care and coordination. The regions own, manage, and finance hospitals. They also finance the majority of services delivered by private general practitioners (GPs), office-based specialists, physiotherapists, dentists, and pharmacists, as well as specialized rehabilitation. Eighty percent of funding for the regions comes from the state, and 20 percent from municipalities.
Municipalities are responsible for financing and delivering nursing home care, home nurses, health visitors, some dental services, school health services, home help, substance use treatment, public health and health promotion, and general rehabilitation.
The general regulation, planning, and supervision of health services, including overall cost-control mechanisms, take place at the national level through Parliament, the Ministry of Health, and four governmental agencies:
- The Health Authority, which provides general monitoring and regulation of quality through such measures as clinical guidelines and licensing of health care personnel, usually in close collaboration with representatives from medical societies
- The Medicines Agency, which regulates market access and pharmacovigilance, among other functions
- The Patient Safety Authority, which handles patient complaints and compensation claims, collects information about errors to foster systematic learning, and provides information about treatment abroad
- The Health Data Authority, which handles data collection and infrastructure
- The Danish Agency for Patient Complaints.
National authorities also have important roles in planning the location of specialist services, approving regional hospital plans, and approving mandatory health agreements between regions and municipalities to coordinate service delivery. In addition, the Health Data Agency provides online access to benchmarking data related to service, quality, and number of treatments performed, as well as data from clinical registries and information about pharmaceutical prices and reimbursement levels.1
Danish Regions and Local Government Denmark negotiate economic agreements on behalf of regions and municipalities and participate in monitoring agreed-upon performance targets. They also play important roles in collecting and sharing knowledge to facilitate development and implementation.
Organized patient groups engage in policymaking at the national, regional, and municipal levels.
Role of public health insurance: Public expenditures accounted for 84 percent of total health spending in 2016, representing 8.7 percent of GDP. Overall, health care expenditures represented 10.4 percent of GDP.2 It should be noted that Denmark includes long-term care services in its accounting for total health care spending, unlike other Organisation for Economic Co-operation and Development (OECD) countries.3
Health care is financed mainly through a progressive national income tax. The national government allocates heath care funding to regions and municipalities, mostly as block grants, with amounts adjusted for demographic and social differences. These grants finance 77 percent of regional health functions. A minor portion of state funding for regional and municipal services is tied to specific priority areas and targets, usually defined in the annual economic agreements between the national government and the municipalities or regions. Current targets incentivize a continued transition from hospital-based care to primary care and home-based care. The remainder of financing for regional services comes from municipal activity-based payments, which are financed through a combination of municipal progressive income taxes and state block grants.
Role of private health insurance: Complementary voluntary health insurance, purchased on an individual basis, covers statutory copayments — mainly for pharmaceuticals and dental care — and services not fully covered by the state, such as physiotherapy. Some 2.45 million Danes (42%) have such coverage, which is provided almost exclusively by the nonprofit organization Danmark.4
In addition, nearly 1.69 million Danes (30%) hold supplementary insurance to gain expanded access to private providers, mostly for physiotherapy and minor elective surgeries.5 Seven for-profit insurers sell policies, which are provided mainly through private employers as a fringe benefit, although some public-sector employees are also covered. Students, pensioners, the unemployed, and others outside the job market are generally not covered by supplementary insurance.
Private expenditures accounted for nearly 16 percent of health care spending in 2016.6
Services covered: The national, publicly financed health care system fully covers the following services:
- primary and preventive care
- specialist care
- hospital care, including inpatient prescription drugs
- mental health care
- long-term care
- dental services for children under age 18.
Outpatient prescription drugs, adult dental care, physiotherapy, and optometry services are partially covered through subsidies.
Home care is organized and financed by the municipalities. Municipalities also fully finance maternity care, preventive home visits for infants, and consultations for toddlers and preschoolers. Municipalities are also responsible for providing durable medical equipment for citizens with a permanent need. Hospice care is financed and delivered by the regions.
There is no nationally defined benefit package for health care. Decisions about levels of service and new medical treatments are made by the regions, within a framework of national laws, agreements, guidelines, and standards. Municipalities decide on the service level for most other welfare services, including social care, within a framework of national regulation. In practice, most evidence-based treatments are covered. These include fertility treatment (with some limitations) and necessary cosmetic surgery.
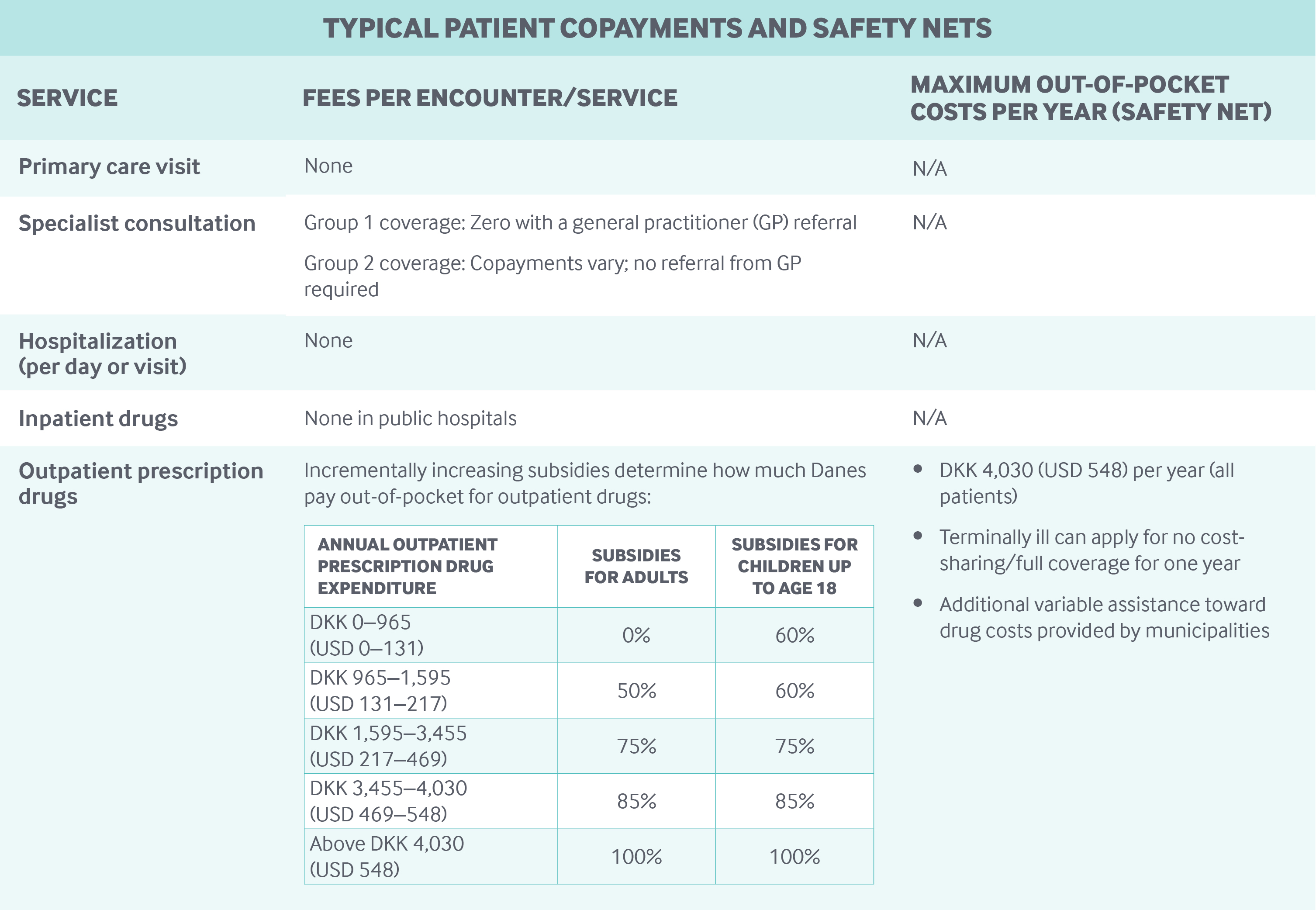
Cost-sharing and out-of-pocket spending: Cost-sharing is applied to adult dental care (coinsurance 35%–60%), outpatient prescriptions, temporary home care, residential long-term care, corrective lenses, and travel vaccinations. There is no cost-sharing for hospital care, primary care services, dental care for children under age 18, childhood immunizations, cancer screenings, maternity care, hospice care, or permanent home care. Only Danes who choose Group 2 insurance coverage owe a copayment when visiting a specialty physician.
Household out-of-pocket payments represented 13.7 percent of total health expenditures in 2016, covering mostly outpatient drugs, corrective lenses, hearing aids, dental care, and payments to private specialists and clinics outside the public referral scheme.7
Safety nets: Because most care is covered under public health insurance, there is limited need for safety nets. Danes receive subsidies for outpatient drugs, and there is a yearly out-of-pocket maximum for drugs (see table).8,9 There are also subsidies for physiotherapy and adult dental care. In addition, the municipalities provide means-tested social assistance to older people for long-term care.
How is the delivery system organized and how are providers paid?
Physician education and workforce: The number of physicians is regulated at the national level through limitations on the number of medical education training positions and the number of practicing physicians per region who can receive public funding. There are four medical schools, all public, offering medical studies lasting six years. None of them charge tuition fees.
In recent years, there has been a shortage of medical providers willing to set up general practices in rural areas. This has led to legislative changes that allow the regions to invite bids for practices or to run the practices as regional units. The regions have also undertaken other initiatives to address the shortage, such as developing programs to attract foreign doctors, providing clinic buildings for free, and allowing doctors to own several clinics. The state has also increased uptake at medical schools.
Primary care: Approximately 22 percent of doctors work in general practice. Almost all GPs are self-employed and are paid by the regions via capitation (about 30% of income) and fee-for-service (70% of income). Rates are set through national agreements with physician associations.
The average income for a GP was DKK 1.1 million (USD 149,500) in 2012, which is about the same as the average salary for senior hospital doctors (specialists).10
The practice structure is gradually shifting from solo to group practices, typically consisting of two-to-four GPs and two-to-three nurses.11 Nurses are paid by the clinics and typically assist in the management of patients with chronic illnesses or complex needs, as well as blood sampling and vaccinations. Multispecialty clinics — with GPs, physiotherapists, and office-based specialists operating out of the same facilities but under separate management — have also been increasing in recent years.
As explained earlier, Danes have a choice of two public health insurance options. Patients who choose Group 1 coverage are required to register with a GP; they have free choice of any available local GP.
GPs cannot charge above the fee schedule for publicly funded patients in Group 1.
Outpatient specialist care: Outpatient specialist care is delivered at hospital-based ambulatory clinics by doctors employed by the hospital or by self-employed specialists in privately owned facilities.
Private self-employed specialists may work full-time or part-time. Part-timers may also work in the hospital sector, subject to codes of conduct, with their activity level monitored and the earnings in their private outpatient clinics limited by the regions.
Self-employed private providers are paid by the regions on a fee-for-service basis for public patients. Fees to private providers are set through national negotiations between regional representatives and physician associations, based on regional priorities and resource assessments.
Private specialists and hospitals also receive out-of-pocket payments from patients and reimbursements by private voluntary insurers. Fees for private (and Group 2) patients are set by the specialists, and may be above the fee schedule. Private practitioners and private hospitals may also receive patients referred from public-sector providers; they are paid for these services through specific agreements with the regions.
Administrative mechanisms for direct patient payments to providers: There is no out-of-pocket payment for primary or specialty care consultations and treatments for patients in Group 1, while drugs prescribed in clinics outside hospitals do incur a copayment when below the annual limit of DKK 4,030 (USD 548). Primary care physicians and specialists are paid directly by the regions when registering provision of services electronically. Group 2 patients make a copayment to supplement the automatic payment by regions.11
After-hours care: After-hours care is organized by the regions. The first line of contact is a regional after-hours telephone service with a GP (or a specialized nurse in the Copenhagen region) triaging to home visits or to an after-hours clinic, which is usually colocated with a hospital emergency department. Information on after-hours patient visits is routinely sent electronically to GPs.
GPs enter collective agreements with regions to provide after-hours care. The GPs are responsible for delivering after-hours care; however, individual GPs have flexibility in taking on more or less responsibility within this scheme, and they receive a higher fee-for-service payment for after-hours care than for normal care. Capitation does not apply to after-hours care.
There are also walk-in emergency units at larger hospitals.
Hospitals: Approximately 97 percent of hospital beds are publicly owned. Private hospitals are relatively small and mostly provide specialty care, such as elective surgery.
Regions decide on budgeting mechanisms, generally using a combination of a fixed budget and activity-based funding based on diagnosis-related groups (DRGs). The fixed budget makes up the bulk of the funding (although significant fluctuations occur among specialties and hospitals). DRG rates are calculated by the Ministry of Health at the national level, based on average costs.
Activity-based funding is usually combined with target levels of activity and declining rates of payment to control expenditures. This strategy succeeded in increasing activity and productivity by an average of 2.4 percent annually from 2003 to 2015.12 Bundled payments are not yet used extensively, but experiments are being carried out in all five regions. Similarly, all five regions are experimenting with various types of value-based payment schemes for select hospitals and departments.
Hospital physicians are salaried and employed by regional hospitals. Physicians employed by public hospitals are not allowed to see private patients within the hospital. Patients can choose among public hospitals, and payment follows the patient to the receiving hospital if the facility is in another region.
Mental health care: Inpatient psychiatric care in public psychiatric hospitals and wards is fully covered by public health insurance without cost-sharing. Outpatient psychiatric care is provided in hospital clinics by salaried hospital staff or in private clinics by privately practicing specialists who receive most of their income through public fee-for-service funding.
Psychologists are employed in hospitals by municipalities, or operate in private practices. Community mental health services are provided by the municipalities, which can contract with a combination of private and public service providers; however, most providers are public and salaried.
Since 2014, Danes have had the right to a diagnostic psychiatric assessment within one month of referral. Treatment must be commenced within two months for less serious conditions and one month for more serious conditions. There are walk-in units for acute psychiatric care in all regions.
Long-term care and social supports: Responsibility for long-term and chronic care is shared between regional hospitals, GPs, and providers of municipal institutional and home-based services. Hospital-based ambulatory chronic care is financed in the same way as other hospital services and is provided to patients who have severe chronic care needs or require specialized rehabilitation services. GPs are responsible for ongoing medical follow-up for most people with chronic care needs, while the municipalities organize, fund, and deliver care and assisted living support at home or in municipal institutions, based on individual needs assessments.
Most municipal long-term care is provided at home, in line with a policy initiative to enable people to remain at home as long as possible. Municipal assisted-living support with ongoing visits is relatively extensive. However, a recent study showed that 46 percent of relatives have provided voluntary assistance to older relatives one-to-two times a week, mostly for shopping, cleaning, cooking, and other practical activities.13 A minority (9%) of relatives also assist in personal care.
The proportion of citizens over age 75 who live in protected housing and nursing homes dropped from 15 percent to 13 percent between 2010 and 2015.14 Home nursing is funded with a medical referral, but temporary home care may be subject to cost-sharing.
Municipalities organize markets to ensure access to both public and private home care providers (personal and practical care, such as cleaning and shopping), and patients may choose between public and private providers. While this system functions relatively well in most municipalities, it has been difficult to attract private providers to remote areas. A considerable number of the elderly choose private providers. Some municipalities also have contracted with private institutions for institutional care of older people, but more than 90 percent of residential care institutions (nursing homes) remain public.
Providers are paid directly by the municipalities, and no cash benefits are paid to patients. Public providers are employed by the municipalities. Most providers are public or private not-for-profit, and a few are private for-profit.15
Relatives of seriously ill individuals are allowed to take paid leaves of absence from their jobs for up to nine months. These can be incremental and may be divided among several relatives. A similar scheme exists for relatives of terminally ill patients who no longer receive treatment.
Hospices, which may be public or private, are organized by the regions and are fully funded by regions and municipalities. GPs or hospitals can refer terminally ill patients to hospice when no further treatment is possible. There is free choice of hospice with a referral.
What are the major strategies to ensure quality of care?
Quality improvement is a major priority area in health policy, as is reflected in the Danish Health Law.
The Danish Institute for Quality and Accreditation in Healthcare (IKAS) was instrumental in implementing accreditation in hospitals and in primary and municipal health care through the Danish Healthcare Quality Program.16 The program, in operation between 2004 and 2015, was phased out for hospitals and replaced by a new system in which regions are responsible for developing schemes that enable them to meet eight national quality targets and related indicators. These targets have been decided in negotiated agreements between the state, the Danish Regions, and Local Government Denmark. Regional performance on the targets is monitored and published annually.17 Accreditation for primary care is gradually being replaced by a system of collegial collaboration based on quality data. Accreditation is still available for municipal health services on a voluntary basis.
Other transparency efforts are underway. The Ministry of Health, the Ministry of Finance, and the Danish Regions regularly publish comparative-effectiveness (productivity) studies, which help regions and hospital managers benchmark individual hospital department performance.18 Quality data for a number of treatment areas are also captured in clinical registries and made available to institutions (but not individual health providers at the hospital level) through the national online health portal, www.esundhed.dk.19 In addition, patient experiences are collected through biannual national, regional, and local surveys.
To reduce variation in care quality, the Danish Health Authority has laid out standard treatment pathways, with priorities including chronic disease prevention and follow-up interventions. Pathways for 34 cancers have been in place since 2008, covering nearly all cancer patients. The Health Authority monitors the pathways and the speed with which patients are diagnosed and treated. National guidelines and reference programs also enforce the use of pathway programs and national clinical guidelines for all major disease types. The regions develop more specific practice guidelines for hospitals and other organizations, based on general national recommendations.
There are no explicit national economic incentives tied to quality, but all five regions are experimenting with such schemes by including indicators related to waiting times, adherence to guidelines, readmission rates, and patient satisfaction in the evaluation structure. In general, regions are obliged to act in the event of poor results. The Danish Health Authority can step in if regions fail to live up to standards.
Nursing homes and home care agencies are subject to quality inspections by the municipalities and by the Danish Patient Safety Authority. Results of municipal inspections are typically published online, while the authority publishes thematic overview reports on its risk-based inspections.
What is being done to reduce disparities?
Equity is a value in the Danish health care system, as in other Nordic welfare systems. This is evident in the key principle of equal and easy access in the Danish health law and, more broadly, as an underlying argument for universal, tax-financed health systems that provide coverage to all citizens largely free of charge. Equity is also a key focus for regional and municipal organizers of health and social care services. Nevertheless, some social and geographical differences in health remain.
One of the key mechanisms for ensuring geographical equity in health care is a scheme for systematic redistribution of tax revenues from affluent to less affluent municipalities based on sociodemographic parameters. Equity aims are also supported by various efforts to standardize treatment quality through pathway programs and mandatory publication of relevant indicators for comparison across geographical units. Finally, the implementation of nationwide free choice of hospitals and maximum waiting times for hospital diagnosis and treatment also pressures the regions to deliver fast and equitable access.
The Danish Health Agency regularly publishes reports on variations in health and health care access based on survey data, subdivided according to age, gender, education, employment, and geography (region).20 The reports have prompted the formulation of municipal-level action plans and initiatives, including:
- Targeted interventions to promote smoking cessation
- Prohibition of the sale of strong alcohol to young people
- Establishment of anti-alcohol policies in all educational institutions
- Further encouragement of municipal disease-prevention activities, such as through increased municipal cofinancing of hospitals, which creates economic incentives for municipalities to keep citizens healthy and out of the hospital
- Improved psychiatric care
- A mapping of health profiles in all municipalities, to be used as a tool for targeting municipal disease-prevention and health-promotion activities
- Various projects and special funding opportunities, for example, those focusing on the health of socially disadvantaged groups such as the immigrants and ethnic minorities.
What is being done to promote delivery system integration and care coordination?
Mandatory health agreements between the municipalities and regions related to coordination of care address a number of topics related to admission and discharge from hospitals, rehabilitation, prevention, psychiatric care, information technology (IT) support systems, and formal progress targets. Agreements are formalized for municipal and regional councils at least once per four-year election term, and generally take the form of shared standards to guide improvements in different phases of a patient’s journey; these agreements must be approved by the Danish Health Authority. The degree to which the regions and municipalities succeed in reaching agreed-on goals is measured by national indicators published online.21
The agreements are partially supported by IT systems with information that is shared among caregivers. All GPs use electronic information systems as a conduit for discharge letters, electronic referrals, and prescriptions. In addition, all health care personnel have access to a shared database of prescriptions, known as the shared medical card.
The national indicators are also important in a new (2019) national scheme for allocation of funding from the state to the regions. The scheme incentivizes further transition from hospital care to primary and home-based care and further development of digitally supported and integrated care by making part of the national funding contingent upon five general criteria:
- Fewer hospital admissions per citizen
- Less in-hospital treatment for chronic care patients
- Fewer unnecessary readmissions within 30 days
- Increased use of telemedicine
- Better integration of IT across regional and municipal sectors.
Regions and municipalities have implemented various measures to promote care integration. Examples include:
- The use of outreach teams from hospitals conducting follow-up home visits
- Training programs for nursing and care staff
- The establishment of municipal units located within hospitals to facilitate communication, particularly in regard to discharge
- Shared municipal and hospital nurses
- The use of general practitioner practice coordinators.
Many coordination initiatives place an emphasis on people with chronic care needs, multiple morbidities, or frailty resulting from aging or mental health conditions.22 The municipalities are in charge of a range of services, including social care, elder care, and employment services; most are currently working on models for better integration of these services, such as joint administration with shared budgets and formalized communication procedures.
Practices increasingly employ specialized nurses, and several municipalities and regions have set up joint multispecialty facilities, commonly called health houses. Models vary, but often include GPs, practicing specialists, and physiotherapists, among others. The system of enlistment with a particular GP serves to develop long-standing relationships and to strengthen the role of GPs as coordinators of care for patients based on a comprehensive view of their patients’ individual needs regarding prevention and care.
What is the status of electronic health records?
IT is used at all levels of the health system as part of a national strategy supported by the National Agency for Health IT. Each of the five regions uses electronic health record (EHR) systems for hospitals, with adherence to national standards for compatibility. All citizens in Denmark have a unique electronic personal identifier that is used in all public registries, including health databases. The government has implemented an electronic medical card storing encoded information about each patient’s prescriptions and medication use; this information is accessible by the patient and all relevant health professionals.
General practitioners also have access to an online medical handbook with updated information on diagnosis and treatment recommendations. Two regions are currently implementing a comprehensive new EHR and data capture system developed by EPIC. While the initial implementation has been problematic, it is expected to provide benefits in the long run. The three other regions are using a system developed by Systematic. Shared standards facilitate communication between the two IT systems at the general level, but with a number of challenges at the detailed clinical level.
The national health information portal, Sundhed.dk, offers differentiated access for health staff and the wider public.23 It provides general information on health and treatment options and access to individuals’ own medical records and history. For professionals, the site serves as an entry to medical handbooks, scientific articles, treatment guidelines, hospital waiting times, treatments offered, and patients’ laboratory test results. The portal also serves as a communication platform for referral, discharge, and prescription information among primary care providers, regions, hospitals, and pharmacies.
How are costs contained?
The overall framework for controlling health care expenditures is outlined in a budget law, which sets budgets for regions and municipalities and specifies automatic sanctions if budgets are exceeded. The budget law is supplemented by annual agreements between regional, municipal, and state governments to coordinate policy initiatives aimed at limiting spending, including direct controls of supply.
The performance of the regions is monitored in terms of activity and a number of quality measures. The results are published and form a central part of the governance relations between state and regions. As of 2019, part of the regional funding is dependent on the regions addressing specific criteria related to coordination and integration of care. In addition, a minor portion of the funding will be withheld and redistributed to technology development projects. The aim is to pressure the regions to further increase productivity.
At the regional level, hospital cost control includes a combination of global budgets and activity-related incentives (see “ Hospitals”).
Inpatient pharmaceutical expenditures are controlled through national guidelines and clinical monitoring combined with collective purchasing. The purchase of hospital medicines takes place through tendering and price negotiations by the joint regional organization Amgros.
A new regional medicines council was established in 2017 to provide information to Amgros and other decision-makers on the cost-effectiveness of new pharmaceuticals. The council evaluates the clinical effectiveness of new pharmaceuticals and provides input to Amgros, which negotiates prices with providers of pharmaceutical products. The ensuing joint evaluation of effectiveness and costs leads to a decision on whether or not to recommend that regions adopt the drug as standard treatment. The council has finished the evaluation of 41 applications for new drugs or changes in the use of drugs since 2017. In 25 cases, the council recommended the drug as a possible standard treatment in regional hospitals; 13 requests were rejected; and for three drugs, the recommendation was to use the drug as standard treatment for some patient groups but not for others.
In September 2018, the Danish government signed an agreement with the Norwegian government to facilitate joint tenders for hospital drugs and information-sharing about new pharmaceuticals.24 The collaboration with Norway also aims to increase access to generic pharmaceuticals in the two markets.
Finally, in a 2019 legislative proposal, the government has announced plans to introduce a new external reference pricing system for drugs that are outside the agreement with the pharmaceutical companies.28 Reference prices from nine European countries will be used to calculate the maximum list price in Denmark. This scheme supplements the existing agreement with the Danish Association of the Pharmaceutical Industry (Lif), which applies a decrease of 10 percent to the list prices of hospital drugs from 2016 to 2019.25
Policies to control outpatient pharmaceutical expenditures include generic substitution, prescribing guidelines, and assessments by the regions of prescribing behavior deviations. Pharmaceutical companies report a monthly price list to the Danish Health Authority, and pharmacies are obliged to choose the cheapest alternative with the same active ingredient, unless a specific drug is prescribed. Patients may choose more expensive drugs, but they have to pay the difference.
Collective agreements with general practitioners and specialists include various clauses about rate reductions if overall expenditures exceed given levels. Regions also monitor the number and type of consultations and may intervene if levels deviate significantly from the average.
Health technology assessments are developed within European Union networks and at the regional level for hospital-level procedures and technology decisions. These assessments, as well as cost-effectiveness information, guide decision-making on new treatments and guidelines.
Regions may enter into contracts with private providers to deliver diagnostic and curative procedures. Prices for those services are negotiated between regions and private providers and can be lower than rates in the public sector.
Together, these measures have been relatively successful in controlling expenditures and driving up activity levels. The average annual productivity in the hospital sector increased by 2.3 percent from 2003 to 2016. During the same period, standardized hospital mortality rates declined and high patient satisfaction rates were maintained.26,27
What major innovations and reforms have recently been introduced?
- A 2018 agreement with Norway will facilitate joint tenders for hospital drugs and information-sharing about new pharmaceuticals (see “How are costs contained?”).
- A new external reference pricing system for drugs will be implemented in 2020 (see “How are costs contained?”).
- The central government and the regions have entered an agreement to restructure the financing of the regions. The previous requirement of an annual 2 percent productivity increase for hospitals will be replaced by a funding scheme that holds regions accountable for addressing specific criteria related to coordination and integration of care. In addition, a minor portion of funding will be redistributed to technology development projects.

