By Joost Wammes, Niek Stadhouders, and Gert Westert, Radboud University Medical Center
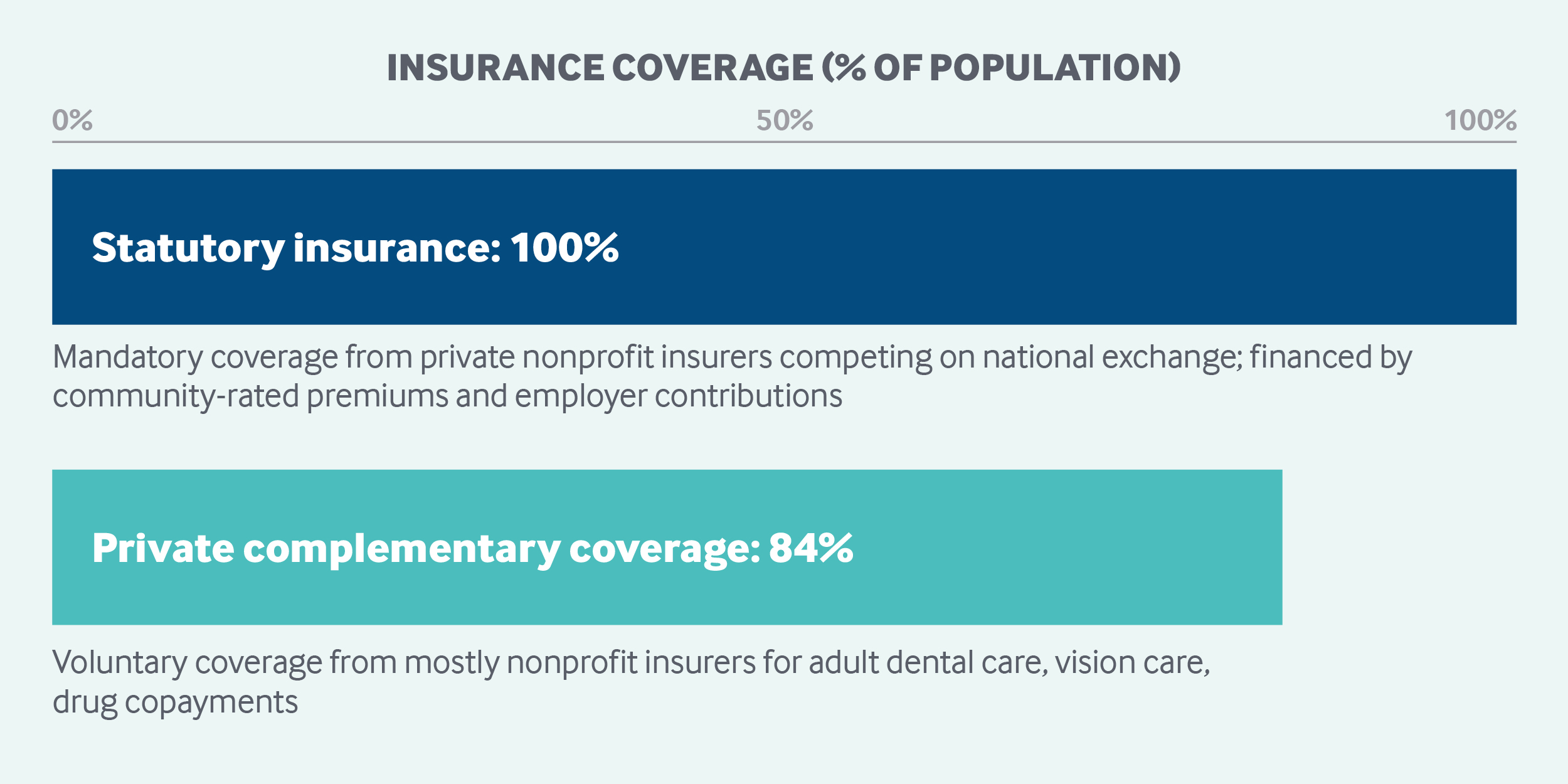
The Netherlands’ universal social health insurance approach merges public and private insurance. All residents are required to purchase statutory health insurance from private insurers, which are required to accept all applicants. Financing is primarily public, through premiums, tax revenues, and government grants. The national government is responsible for setting health care priorities and monitoring access, quality, and costs. Standard benefits include hospital, physician, home nursing, and mental health care, as well as prescription drugs. Adults pay premiums, annual deductibles, and coinsurance or copayments on select services and drugs. The government pays for children’s coverage up to age 18.
Sections
How does universal health coverage work?
In the Netherlands, a national health insurance program was first rolled out in 1941, reflecting the German Bismarck model of public and private health insurers.1 Around 63 percent of the population was covered by public health insurance, while the more affluent could opt for private insurance or choose to remain uninsured.
At the turn of the century, concerns over inefficiencies and long waiting lists provided momentum for market-oriented reform based on the managed competition model proposed by American economist Alain C. Enthoven.2 The 2006 Health Insurance Act merged the traditional public and private insurance markets into one universal social health insurance program underpinned by private insurance and mandatory coverage.
All residents (and nonresidents who pay Dutch income tax) must purchase statutory health insurance from private insurers. Adults choose a policy on an individual basis (no family coverage), and children under 18 are then automatically covered. Insurers are required to accept all applicants, and enrollees have the right to change their insurer each year.
The uninsured are fined, and their insurance premiums may be levied directly from income. People who conscientiously object to insurance can opt out by making mandatory contributions into a health savings account. Active members of the armed forces (who are covered by the Ministry of Defense) are exempt.
Undocumented immigrants cannot purchase health insurance and have to pay for most treatments out-of-pocket (excluding acute care, obstetric services, and long-term care). However, some mechanisms are in place to reimburse costs that undocumented immigrants are unable to pay. Political asylum–seekers fall under a separate, limited insurance plan. Permanent residents living in the Netherlands for more than three months are obliged to purchase private insurance. Short-term visitors are required to purchase insurance for the duration of their visit if they are not covered through their home country.
Since 2011, the number of uninsured in the Netherlands has steadily declined. At the end of 2016, 23,000 people (less than 0.2% of the population) remained uninsured.
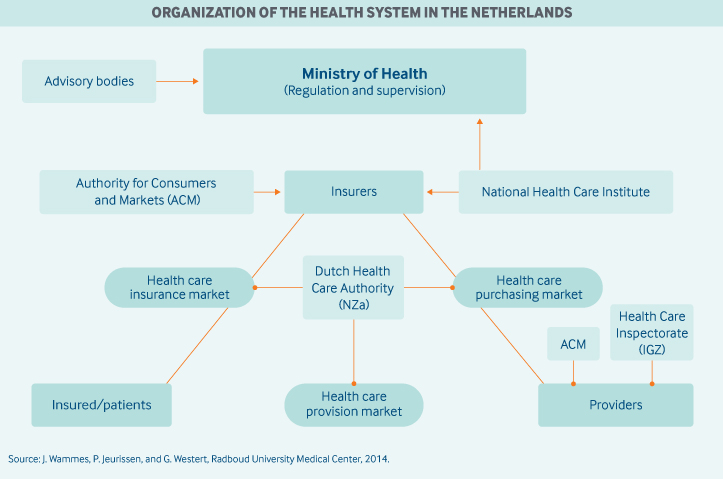
Role of government: The national government has overall responsibility for setting health care priorities; introducing legislative changes when necessary; and monitoring access, quality, and costs in the country’s market-based system.
The municipalities are responsible for overseeing some health care services, including preventive screenings and outpatient long-term services. The federal Ministry of Health’s role is to safeguard health care from a distance rather than managing it directly.
A number of arm’s-length (independent) agencies are responsible for setting operational priorities:
- At the national level, the Health Council advises government on evidence-based medicine, health care, public health, and environmental protection.
- The Medicines Evaluation Board oversees the efficacy, safety, and quality of medicines.
- The National Health Care Institute assesses new technologies for efficacy and cost-effectiveness, and advises the Ministry of Health on whether to include those technologies in the mandatory benefit package.
- The Dutch Health Care Authority (Nederlandse Zorgautoriteit) has primary responsibility for ensuring that the health insurance, health care purchasing, and care delivery markets all function appropriately.
- The Dutch Competition Authority (Autoriteit Consument en Markt) enforces antitrust laws among both insurers and providers.
- The Health Care Inspectorate supervises the quality, safety, and accessibility of care. Self-regulation by medical doctors is also an important aspect of the Dutch system.3
- Health information technology (IT) is not centralized in one body. The Union of Providers for Health Care Communication (Vereniging van Zorgaanbieders voor Zorgcommunicatie) is responsible for the exchange of data via an IT infrastructure.
Role of public health insurance: In 2016, the Netherlands spent 10.5 percent of its GDP on health care, and 81 percent of spending was collectively financed through a combination of earmarked payroll taxes paid by employers (46%), general taxation (22%), insurance premiums paid by individuals (21%), and copayments (11%).4
Statutory health insurance is financed partially through a nationally defined annual income tax at 6.9 percent of income up to EUR 54,614 (USD 69,989).5 The income tax accounts for 45 percent of funding.6
Insurance premiums for individuals, which are determined separately by each insurer, account for another 45 percent of funding. Each insurer sets a premium that applies to all of its enrollees, regardless of their age or health status. However, through employer collectives, lower premiums may be offered.
A government grant for children and adolescents under age 18 provides the remaining 5 percent of financing.
Income taxes and government grants are collected in a central health insurance fund and redistributed among insurers in accordance with a risk-adjusted capitation formula that considers age, gender, labor force status, region, and health risk (based mostly on past drug and hospital utilization).
Private, statutory insurers are expected to engage in strategic purchasing, and contracted providers are expected to compete on both quality and cost. There were 10 statutory insurers in 2018, but the insurance market is dominated by the four largest insurance conglomerates, which account for 90 percent of all enrollees. Currently, all insurers are mandated to operate as nonprofits.
Role of private health insurance: In addition to statutory coverage, most of the population (84%) purchases supplementary voluntary insurance covering a range of services not covered by statutory insurance, such as dental care, alternative medicine, physiotherapy, eyeglasses and lenses, and contraceptives, while also reducing copayments for nonformulary medicines.
Premiums for voluntary insurance are not regulated; insurers are allowed to screen applicants for risk factors. Nearly all of the insured purchase their voluntary benefits from the same (mostly nonprofit) insurer that provides their statutory health insurance.
People with voluntary coverage do not receive faster access to any type of care, nor do they have increased choice among specialists or hospitals. In 2016, voluntary insurance accounted for 7 percent of total health spending.7
Services covered: The government determines the statutory benefit package, and health insurers are legally required to provide the standard benefits. The mandatory benefit package includes:
- care provided by general practitioners (GPs)
- specialty care
- hospital care
- maternal care
- dental care up to age 18
- prescription drugs
- physiotherapy up to age 18
- home nursing care
- a limited number of health promotion programs, including those for smoking cessation and some weight management advice
- basic ambulatory mental health care for mild-to-moderate mental disorders
- specialized outpatient and inpatient mental care for complicated and severe mental disorders.
Some treatments, such as general physiotherapy, are only partially covered for some people with specific chronic conditions. Some elective procedures are excluded, such as cosmetic plastic surgery without a medical indication, dental care after age 18, and vision care without medical indication. A range of medical devices are covered, including hearing aids and orthopedic shoes, but wheelchairs and other walking aids are excluded.
Prevention and social supports are not covered by statutory health insurance but are financed through general taxation. The Public Health Act describes municipal responsibilities for national prevention programs, vaccinations, and infectious disease management. Municipalities can install additional prevention programs, such as healthy living and obesity reduction programs, but the provision of such services can vary widely from one municipality to another.
Long-term care is financed separately from statutory health insurance (see the long-term care section below).
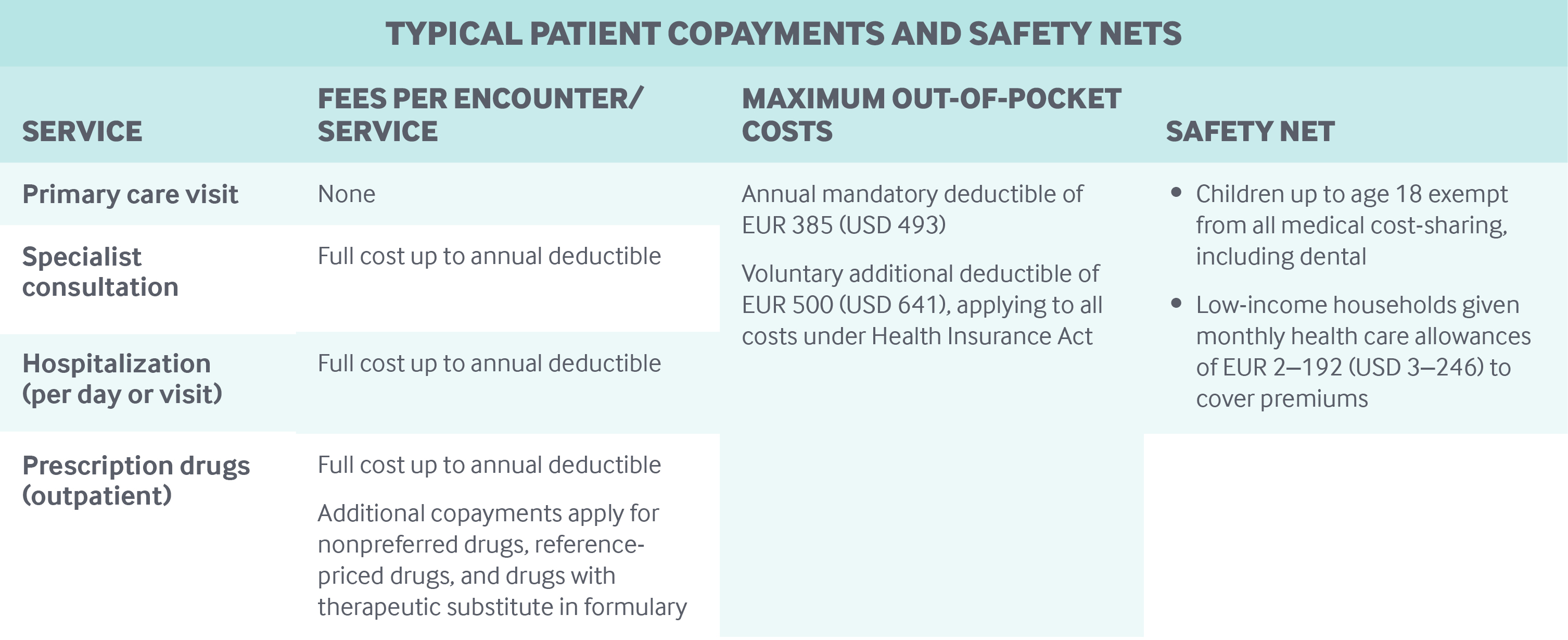
Cost-sharing and out-of-pocket spending: In the statutory health insurance system, the main form of cost-sharing is a mandatory deductible, which was EUR 385 (USD 493) in 2019. In addition, consumers may pay a voluntary deductible of EUR 500 (USD 641), on top of the mandatory deductible, in exchange for a lower monthly premium. People pay the full cost of specialty and hospital care up to the deductible. The deductible covers a broad range of services, including hospital admissions, specialist services, and prescription drugs. GP care, preventive services (including most immunizations and breast cancer screenings), and children’s health care are provided for free.
Copayments, coinsurance, or direct payments may be required even after the deductible is met for some selected services, such as nonformulary medications, physiotherapy for adults, medical transportation, and medical devices. In addition, patients with restricted network plans who visit providers that do not have contracts with the insurer may be required to pay up to 25 percent of the cost of that out-of-network care.
Safety nets: In addition to providing free primary and pediatric care, the government offers means-tested subsidies (health care allowances) to help cover insurance premiums for low-income people. As of 2019, singles must have annual incomes under EUR 29,500 (USD 37,805), and households must have incomes under EUR 38,000 (USD 48,698).8
More than 5 million people (approximately 30% of the population) receive these allowances,9 which are set on a sliding, income-based scale, up to a maximum of EUR 99 (USD 127) per month for singles and EUR 192 (USD 246) per month for households.10
How is the delivery system organized and how are providers paid?
Physician education and workforce: The number of medical doctors is regulated through caps on the number of medical students, at both a national and a university level. Medical schools are located in private, nonprofit university medical centers. Medical students pay a yearly tuition fee of approximately EUR 2,100 (USD 2,691). The Capacity Body (Capaciteitsorgaan) advises the Ministry of Health on all specialized postgraduate training programs for medical specialists to ensure that supply matches demand.
There are no national initiatives to ensure an adequate supply of medical providers in rural or remote areas. In rural areas, GPs may assume the role of pharmacists.11
Primary care: In 2017, there were 13,364 registered primary care doctors (GPs) and 23,236 medical specialists.12,13 Eighty-two percent of these physicians worked in small practices of two to seven physicians in 2016; 18 percent worked in solo practices.14
Most GPs work independently or in a self-employed partnership; one-third are employed by or have a short-term contract with a practice owned by another GP.15
The GP is the central figure in Dutch primary care. The typical practice size is approximately 2,200 patients per full-time working GP. Although registration with a GP is not formally required, most citizens (over 95%) are registered with one they have chosen, and patients can switch GPs as often as they like. GPs have a gatekeeping function; referrals are required for both hospital and specialist care.16
Many GP practices employ salaried nurses and primary care psychologists. Reimbursement for primary nursing care is received by the GP, so any productivity gains that result from substituting a nurse for a doctor accrue to the GP.
Chronic care management is coordinated through care groups, which are mostly GP networks. Care groups are legal entities that assume clinical and financial responsibility for enrolled chronic disease patients. The groups purchase services from multiple providers. To incentivize care coordination, bundled payments are provided for certain chronic diseases, such as diabetes, cardiovascular conditions, and chronic obstructive pulmonary disease (COPD).
In 2015, the government introduced a new GP funding model17 comprising three segments:
- Segment 1 (approximately 75% of GP spending) funds core primary care services and consists of a capitation fee per registered patient, consultation fees for GPs (including phone consultations), and consultation fees for ambulatory mental health care at the GP practice. The Dutch Health Care Authority (Nederlandse Zorgautoriteit) determines national provider fees for this segment.
- Segment 2 (approximately 15% of GP spending) consists of funding for programmatic multidisciplinary care for diabetes, asthma, and COPD, as well as for cardiovascular risk management. Prices are negotiated with insurers.
- Segment 3 (approximately 10% of GP spending) provides GPs and insurers with the opportunity to negotiate additional contracts that encourage innovation and tie payment to performance.
Primary care providers are not allowed to bill patients above the fee schedule.
In 2018, self-employed GPs earned an average gross annual income of EUR 135,000 (USD 173,004), excluding after-hours care. In comparison, in 2016, maximum gross annual incomes of specialists were estimated at EUR 160,000 (USD 205,042) for salaried specialists, and EUR 211,000 (USD 270,399) for independent specialists.18 The ratio of specialists to GPs was 1.7:1 in 2017.19,20
Outpatient specialist care: Nearly all specialists are hospital-based and either are part of a group practice (39%) or are on salary, mostly in university clinics (49%). The remaining 12 percent worked both on salary and independently in 2015.21
As of 2015, specialist fees are freely negotiable between independent specialist associations and hospitals. This so-called integral funding dramatically changed the relationship between medical specialists and hospitals. Hospitals now have to allocate their financial resources among their specialists.
After patients receive a referral for specialist treatment (in any hospital), they are free to choose their provider, but insurers may set different conditions, like cost-sharing, for choosing certain specialists.22
In 2016, there were 229 independent private and nonprofit outpatient treatment centers whose services were limited to same-day admissions for nonacute, elective care (such as orthopedic surgery) covered by statutory insurance.23
Administrative mechanisms for direct patient payments to providers: Regular GP visits are free of charge, being exempt from the deductible. Patients generally do not pay specialists directly. Instead, the annual deductible is paid to the insurer. The insured has the option of paying the deductible before or after receiving health care and may choose to pay all of the deductible at once or in installments. Copayments, such as those for drugs or transportation, have to be paid directly to the provider.
After-hours care: After-hours care is organized at the municipal level in “GP Posts,” which are walk-in centers, typically run by a nearby hospital, that provide primary care between 5:00 p.m. and 8 a.m. Nearly all GPs work for a GP Post. They must provide at least 50 hours of after-hours care annually to maintain their registration as GPs.
Specially trained medical assistants answer the phone and perform triage; GPs decide whether patients need to be referred to a hospital. Doctors are compensated separately at hourly rates for after-hours care and house calls (on top of their regular income).
The GP Post sends information regarding a patient’s visit electronically to the patient’s regular GP. Since after-hours care is typically provided at hospitals, there is no national medical telephone hotline advising patients on their nearest after-hours locations.
Hospitals: In 2018, there were 71 hospital organizations, including eight university medical centers.24 All hospitals are private entities, but profits may not be distributed to shareholders, making the hospital market virtually 100 percent nonprofit.
Hospital payment rates are determined mostly through negotiations between insurers and hospitals over prices, quality, and volumes. The great majority of payments take place through the case-based, diagnosis-treatment combination (DBC) system, which is similar to a diagnosis-related group approach. In 2012, the number of DBCs was reduced from 30,000 to 4,400 to reduce administrative complexity.
The rates for approximately 70 percent of DBCs can be negotiated by providers and insurers. The remaining 30 percent are set nationally by the Dutch Health Care Authority.
Since 2015, independent medical specialist groups have negotiated physician payments with hospitals. Diagnosis–treatment combinations cover both outpatient and inpatient care, as well as specialist costs, strengthening the integration of specialist care within the hospital organization.
A small part of hospital care is reimbursed through so-called add-ons. Add-ons are separate payments that have been developed for the reimbursement of expensive drugs and intensive care unit admissions. In addition, university medical centers receive special allowances for the adoption of new technologies.
Mental health care: Mental health care for mild-to-moderate mental disorders is provided by specially trained psychologists, nurses, and social caregivers in basic ambulatory care settings, such as GP offices. In cases of complicated and severe mental disorders, GPs will often refer patients for specialized mental health care.
Outpatient mental health care is generally covered as part of the basic statutory benefit package. In contrast, inpatient mental health care is covered as part of the Long-Term Care Act of 2015 (see next section). Hospitals provide acute mental health care.
E-health applications are used widely in mental health care. The government stimulates the use of e-health through various programs, including a EUR 90 million (USD 115 million) investment fund in 2019.25
Long-term care and social supports: In the Netherlands, long-term care and social support programs are separate from but complementary to the curative health system. Long-term care is financed through the Long-Term Care Act (Wet langdurige zorg) of 2015, a statutory social insurance scheme for long-term care and otherwise uninsurable medical risks and costs that cannot be reasonably borne by individuals. To fund long-term care insurance, taxpayers contributed 9.65 percent of their taxable income up to EUR 33,791 (USD 43,304) in 2017.26
Long-term care encompasses residential care, personal care, supervision, medical care, and nursing care, as well as medical aids and transport services. Patients in need of permanent supervision or who need assistance 24 hours a day to prevent escalation or serious harm are eligible for long-term care benefits. The Center for Needs Assessment (Centrum Indicatiestelling Zorg), a governmental agency, determines eligibility based on clinical need alone (no means-testing). In 2016, 314,220 people used long-term care.27
A total of EUR 20 billion (USD 26 billion) was spent on long-term care in 2017, making the Netherlands one of the highest long-term care spenders among countries in the Organisation for Economic Co-operation and Development.28 To reduce spending, some long-term care responsibilities have been transferred to municipalities, with the goal of shifting care from institutional settings to community-based care.
Municipalities receive block grants from the government to cover long-term care expenses. Municipalities have very limited tax-raising abilities.
Municipalities are responsible for ensuring the provision of household services, medical aids, home modifications, services for informal caregivers, preventive mental health care, transport facilities, and other assistance. Municipalities have a great deal of freedom in how they organize long-term care services and in how they support caregivers. In 2017, 1,042,790 people used social support services funded by municipalities.29
Cost-sharing depends on annual income and wealth, age, and household size. For long-term care, an income- and wealth-related copayment up to a maximum of EUR 2,332 (USD 2,988) per month is required.30 For municipal home care and social services, most municipalities require a small income-related copayment.
Long-term care is provided by private, nonprofit organizations. For home care, profits are allowed by law. Home care is provided increasingly by self-organizing nursing units, following the innovative business model of Buurtzorg, a 2007 startup that has increasingly penetrated the Netherlands’ home care market.31
Most palliative care, including hospice care, is integrated into the health system and can be delivered by GPs, home care providers, nursing homes, specialists, and volunteers. Palliative care is financed through a number of sources, but mostly through the Long-Term Care Act.
Personal budgets are provided for patients to buy and organize their own long-term care. In 2016, about 14,200 personal budget holders received on average of almost EUR 20,000 (USD 25,630) annually.32 Personal budgets can be spent on various care and welfare functions, including family caregivers and informal caregivers, although regulations have been tightened.
What are the major strategies to ensure quality of care?
Private, statutory insurers are expected to engage in strategic purchasing, and contracted providers are expected to compete on both quality and cost. At the system level, quality is ensured through legislation governing professional performance, quality in health care institutions, patient rights, and health technologies.
The Dutch Health Care Inspectorate is responsible for monitoring quality and safety. In 2014, the National Health Care Institute was established to further accelerate the process of quality improvement and evidence-based practice. As part of the National Health Care Institute, the National Quality Institute promotes quality measurement and transparency. Most quality assurance is carried out by providers, sometimes in close cooperation with patient and consumer organizations and insurers. There are ongoing experiments with disease management and integrated care programs for the chronically ill.
In the past few years, many parties have been working on quality registries. Most prominent among these are several cancer registries and surgical and orthopedic (implant) registries.
Mechanisms to ensure the quality of care provided by individual professionals include:
- a government-based national registry certifying completion, every five years, of compulsory continuous medical education
- regular on-site peer assessments by professional bodies
- professional clinical guidelines, indicators, and peer review.
The main methods used to ensure quality in hospitals, nursing homes, and other health care institutions include:
- voluntary accreditation and certification granted by independent organizations
- compulsory and voluntary performance assessments based on indicators
- national quality-improvement programs.
Furthermore, quality of care is supposed to be enhanced by selective contracting. For example, insurers should contract only with providers that meet minimum standards for volumes of procedures performed.
Patient experiences are tracked primarily through the Commonwealth Fund’s regularly conducted international health policy surveys,33 but are otherwise not systematically assessed. Although progress has been made, public reporting on quality of care and provider performance is still in its infancy in the Netherlands. Patients may report individual experiences with health care providers and institutions in any sector to the website Zorgkaartnederland.nl on a voluntary basis. Furthermore, several websites provide comparative information about institutions and providers (including hospitals and nursing homes), based primarily on quality indicators obtained from the National Quality Institute and the Dutch Healthcare Inspectorate.
What is being done to reduce disparities?
Every four years, variations in health accessibility are measured and published in the Dutch Health Care Performance Reports by the National Institute for Public Health and the Environment, focusing on socioeconomic differences such as ethnicity and education. Geographic or regional variation is not measured consistently.34
Socioeconomic health disparities are considerable in the Netherlands, with up to seven years’ difference in life expectancy between the highest and lowest socioeconomic groups. Smoking is still a leading cause of death. Although health disparities are monitored by the National Institute for Public Health and the Environment (part of the Ministry of Health), the government does not have specific policies to overcome them. In 2013, the government decided to cover weight loss advice and smoking cessation programs in the statutory benefit package.35
What is being done to promote delivery system integration and care coordination?
A bundled-payment approach to integrated chronic care is applied nationwide for diabetes, COPD, and cardiovascular risk management (see “Primary care” above). Under this system, insurers pay a single fee to a principal contracting entity, known as the care group, to cover a full range of chronic disease services for a fixed period.
The bundled-payment approach supersedes traditional health care purchasing for the applicable condition and divides the market into two segments: one in which health insurers contract care from care groups, and another in which care groups contract services from individual providers, each with freely negotiable fees.36
Over the last years, a number of pilot studies across the Netherlands have been initiated to improve care integration and coordination, focusing primarily on health and lifestyle improvement, population management, and administrative simplification. For instance, the role of district nurses is currently being strengthened to better coordinate care and help reach vulnerable populations. These initiatives have had varying degrees of success.
What is the status of electronic health records?
Virtually all GPs have a degree of electronic information capacity. For example, they use electronic health records (EHRs) and can order prescriptions and receive lab results electronically. At present, all hospitals have an EHR.
Providers must allow patients access to their own files on request, but few hospitals have standard online access options for patients. Electronic records, for the most part, are not nationally standardized or interoperable between domains of care. In 2011, legislation to install a national EHR system failed in Congress. Since then, the integration of EHR systems among providers has been left to the field.
In 2011, hospitals, pharmacies, after-hours GP cooperatives, and organizations representing GPs set up the Union of Providers for Health Care Communication (Vereniging van Zorgaanbieders voor Zorgcommunicatie), responsible for the exchange of data across various platforms and settings via the National Switch Point (LSP).37 Patients must approve their participation in this exchange, and have the right to withdraw. The LSP uses unique provider identification numbers and patient social security numbers under the oversight of the Central Healthcare Information and Occupation Access Point, a government agency. In practice, use of this system is limited.
Other initiatives have focused on improving data exchange. For example, MedMij is a private organization that develops data standards to ensure that portals, provider systems, and apps can be linked to exchange information securely.
How are costs contained?
The main approach to controlling costs relies on market forces while regulating competition and improving the efficiency of care. In addition, provider payment reforms, including a shift from a budget-oriented reimbursement system to a performance- and outcome-driven approach, have been implemented. In the wake of the 2008 global financial crisis, additional activities have been undertaken to contain costs. Since 2012, health care spending has declined from 10.9 percent to 10.5 percent of GDP.38
In 2011, an agreement signed by the Ministry of Health, all health care providers, and insurers set a voluntary ceiling for the annual growth of spending on hospital and mental health care. When overall costs exceed that limit, the government has the ability to control spending via generic budget cuts. The agreement included an extra 1 percent spending growth allowance for primary care practices in 2014 and 1.5 percent in 2015–2017, provided they demonstrated that their services were a substitute for hospital care. The agreement was renewed in 2018.39
The pharmaceutical sector is generally considered to have contributed significantly to the decrease in spending growth. Average prices for prescription drugs declined in 2014, although less than in previous years, with reimbursement caps for the lowest-price generic contributing to the decrease in average price. Reimbursement for expensive drugs has to be negotiated between hospitals and insurers. There is some concern, however, that this and other factors may limit access to expensive drugs in the near future.
Health technology assessment is gaining in importance, and is used mainly for decisions concerning the benefit package and the appropriate use of medical devices. The management of the basic benefit package also contributes to cost containment. Based on advice by the National Health Care Institute, the Ministry of Health has negotiated lower prices with manufacturers for a range of expensive drugs. The Dutch health minister has formulated an ambitious policy proposal aimed, in part, at limiting the pharmaceutical industry’s power over drug pricing. During the Dutch presidency of the European Union in 2016, the topic was successfully put on the EU agenda, but the effectiveness of the proposed policies remains to be seen.
The annual deductible, which accounts for the majority of patient cost-sharing, has more than doubled between 2008 and 2018, from EUR 170 (USD 218) to EUR 385 (USD 493).40 There are some worries that this increase has led to greater numbers of people abstaining from or postponing needed medical care.
Cost containment has been most severe in long-term care. Since 2013, people with lower care needs are no longer entitled to residential care. In addition, the devolution of services to the municipalities as a result of the 2015 Long-Term Care Act was accompanied by substantial cuts to the available budgets (by almost 10%, on average).
The Federation of University Medical Centers has recently started a program aimed at reducing lower-value services.41 In addition, the Dutch Federation of Medical Specialists launched the “Dutch Choosing Wisely” campaign, which is also aimed at reducing lower-value services.42
What major innovations and reforms have recently been introduced?
Long-term care, including home care, was under separate legislation (the Exceptional Medical Expenses Act) until 2015. In 2015, the major reform placed residential long-term care under the newly created Long-Term Care Act, and transferred home care to the Health Insurance Act (medical home care and home nursing care) and Social Support Act (ancillary home services). The reform program’s main goals were to guarantee fiscal sustainability and universal access in the future and to stimulate greater individual and social responsibility by expanding home-based care and social support as an alternative to institutional long-term care. To that end, the municipalities assumed responsibility for providing home care and social services based on the individual needs of the patient. The devolution of services to the municipalities as a result of the 2015 Long-Term Care Act was accompanied by substantial cuts to the available budgets (on average, almost 10%).
In 2015–2016, initial budget reductions were retracted, and future budget increases of EUR 2.1 billion (USD 2.7 billion) were set aside by the government to alleviate fiscal stress in nursing homes.43
In curative health care, market reform and regulated competition remain somewhat controversial. The government, determined to stimulate competition, has, among other measures, required insurers and providers to assume greater financial risk. The affordability and accessibility of expensive drugs have rapidly become prominent issues.44
As of the date of this report, the Health Insurance Act of 2006 has undergone two evaluations.45 The latest evaluation pointed to an imbalance of power, with providers having an advantage over insurers.
The current government has emphasized providing the right care in the right place, focusing on care networks and cooperation and on strengthening primary care. In 2018, a landmark agreement was reached with more than 70 organizations on a set of preventive measures, including smoking cessation. Other recent policy initiatives are focused on reducing labor shortages in the health sector, addressing loneliness among the elderly, and promoting participation in sports.46 The government is also developing policies to improve the long-term sustainability of health care financing.47

