By Tsung-Mei Cheng, Princeton University
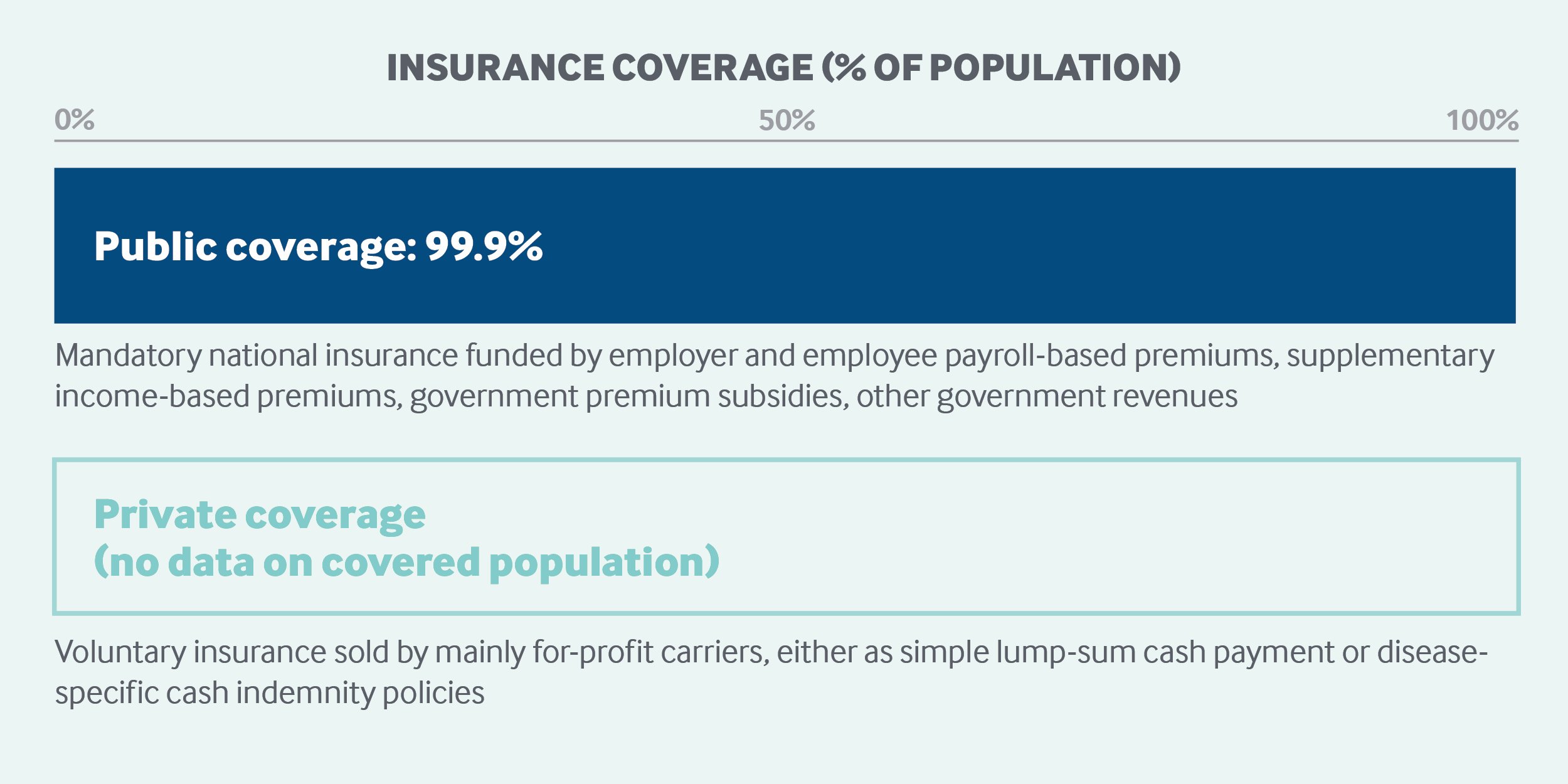
Taiwan’s national health insurance (NHI) provides universal, mandatory coverage. The single-payer system is funded primarily through payroll-based premiums, although the government provides generous premium subsidies for low-income households, civil servants, and others. Health care services are provided mostly by contracted private providers. Covered services include preventive, primary, specialist, hospital, and mental health services. Long-term care, a more recent addition, is provided separately. Out-of-pocket costs include copayments for outpatient care and prescription drugs and coinsurance for hospital stays. Private health insurance consists mostly of disease-specific cash indemnity policies.
Sections
How does universal health coverage work?
Taiwan's NHI system was implemented in 1995. Before then, Taiwan had had more than 10 public insurance schemes, each covering a particular group, such as government employees, farmers, and low-income households. These programs covered 59 percent of the population.1
In 1986, Taiwan's government proposed moving to a universal NHI program. The planning process involved studying health insurance systems abroad, borrowing parts from systems of other countries and adapting them to suit Taiwan's national conditions. On the recommendation of former government adviser Uwe Reinhardt, the late Princeton University economist, Taiwan's government established a single-payer system, which merged Taiwan's then-existing public insurance schemes.2 Reinhardt's recommendation was based on three principles:
- Equity in both access and benefits
- Effective and egalitarian cost control
- Administrative simplicity to help the public understand the system.
The NHI Act became law in July 1994 and implemented rapidly in 1995.3 NHI is a government-run social health insurance program that provides equitable medical and health care services to all in case of illness, injury, and childbirth. Enrollment in NHI is mandatory for all citizens and for foreigners legally residing in Taiwan for longer than six months. Virtually all residents are enrolled.
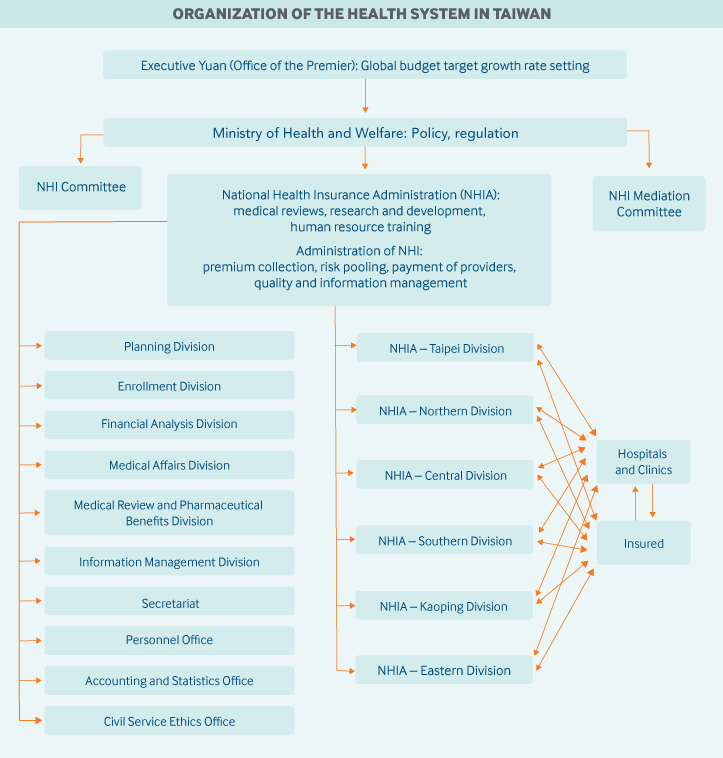
Role of government: The NHI program is administered by the National Health Insurance Administration (NHIA), which falls under the Ministry of Health and Welfare (MoHW). The NHIA is supported by six regional offices connected by a health information infrastructure. Local and municipal governments play little to no role in financing health care.
The bulk of NHI-covered services are delivered through a predominantly private delivery system, although some hospitals are owned and operated by municipal governments.
Because Taiwan has a single-payer health system, governance is fairly simple and straightforward. The MoHW, which sets policy, determines how much the NHI global budget should grow from year to year (subject to approval by the premier’s office) — a months-long process involving multistakeholder negotiations.
The NHIA oversees and administers NHI. The NHIA's main tasks include collecting premiums, risk-pooling, and paying providers, as well as oversight of health services utilization, expenditures, and quality. The NHIA is also responsible for coverage decisions (based on cost-effectiveness analyses of new drugs and treatments), provider fee–setting and fee schedule adjustments, and cost containment. In addition, the agency is charged with identifying new funding sources (such as higher tobacco taxes) and administering a sectoral global budget system.
Parliament plays an important watchdog role in all NHI matters. In addition to its role in negotiating any new health legislation, it must pass an amendment to the NHI Act for any premium rate increases above 6 percent.
Role of public health insurance: Taiwan's national health expenditures totaled 6.4 percent of GDP in 2017, of which NHI accounted for 53.7 percent, representing approximately 3.4 percent of GDP.4
Taiwan’s NHI is a predominantly premium-based social health insurance system. As of 2018, 81 percent of the system’s regular premium revenues are derived in roughly equal measure from individuals, employers, and the government. The balance of revenues comes from supplementary premiums levied on nonpayroll income, such as large bonuses, rent, interest, dividends, professional fees, and income from second and third jobs, as well as additional government premium subsidies, tobacco taxes, and taxes on lottery gains.5
Payroll-based premium payments are made monthly and are calculated as follows:
Salary Basis × Standard Premium (4.69% of payroll × Contribution Ratio ×
(1 + Number of Dependents))
The contribution ratio is based on the insured's “population category status,” which is determined by an individual’s job and by socioeconomic status. For example, employees of “public or privately owned enterprises and organizations” belong to Population Category 1. Their contribution rate is 30 percent of their salary or wage. Of the remainder, 60 percent is paid by their employer and 10 percent by government.
Premium contributions are capped at four members per household (the insured plus three dependents). Any additional household members are covered for free. Both caps and thresholds apply for payroll-based and supplemental premiums.
Role of private health insurance: Private health insurance policies are offered by private for-profit insurers, often as riders to nonmedical policies, such as life or car insurance. These do not cover medical services already covered by NHI, nor do they buy faster access to, or choice of, specialists. Instead, such policies offer disease-specific cash indemnity provisions. Policyholders can use the cash for private hospital rooms or devices, such as drug-eluting stents, not covered by NHI.
As a component of total health expenditures, private coverage is growing. (Precise statistics on private coverage are unavailable.) Many Taiwanese view these policies as savings vehicles.
Services covered: NHI benefits are uniform and comprehensive. Covered benefits include:
- Inpatient and outpatient care (both primary and specialty care)
- Prescription drugs
- Dental care (excluding orthodontics and prosthodontics)
- Traditional Chinese medicine
- Renal dialysis
- Maternity care
- Child delivery
- Physical rehabilitation
- Home care
- Chronic mental health care
- Preventive care, including adult health checkups, cancer screenings, baby and child health care checkups, and childhood immunizations through age 6.
NHI does not cover eyeglasses or visual acuity tests, nor does it cover durable medical equipment such as wheelchairs and hearing aids. It does, however, cover costly cochlear implants for children. Those who need wheelchairs or artificial limbs may apply for government subsidies under the Welfare Law for the Handicapped; veterans who need hearing aids or artificial limbs may receive them free of charge at veterans’ hospitals.6
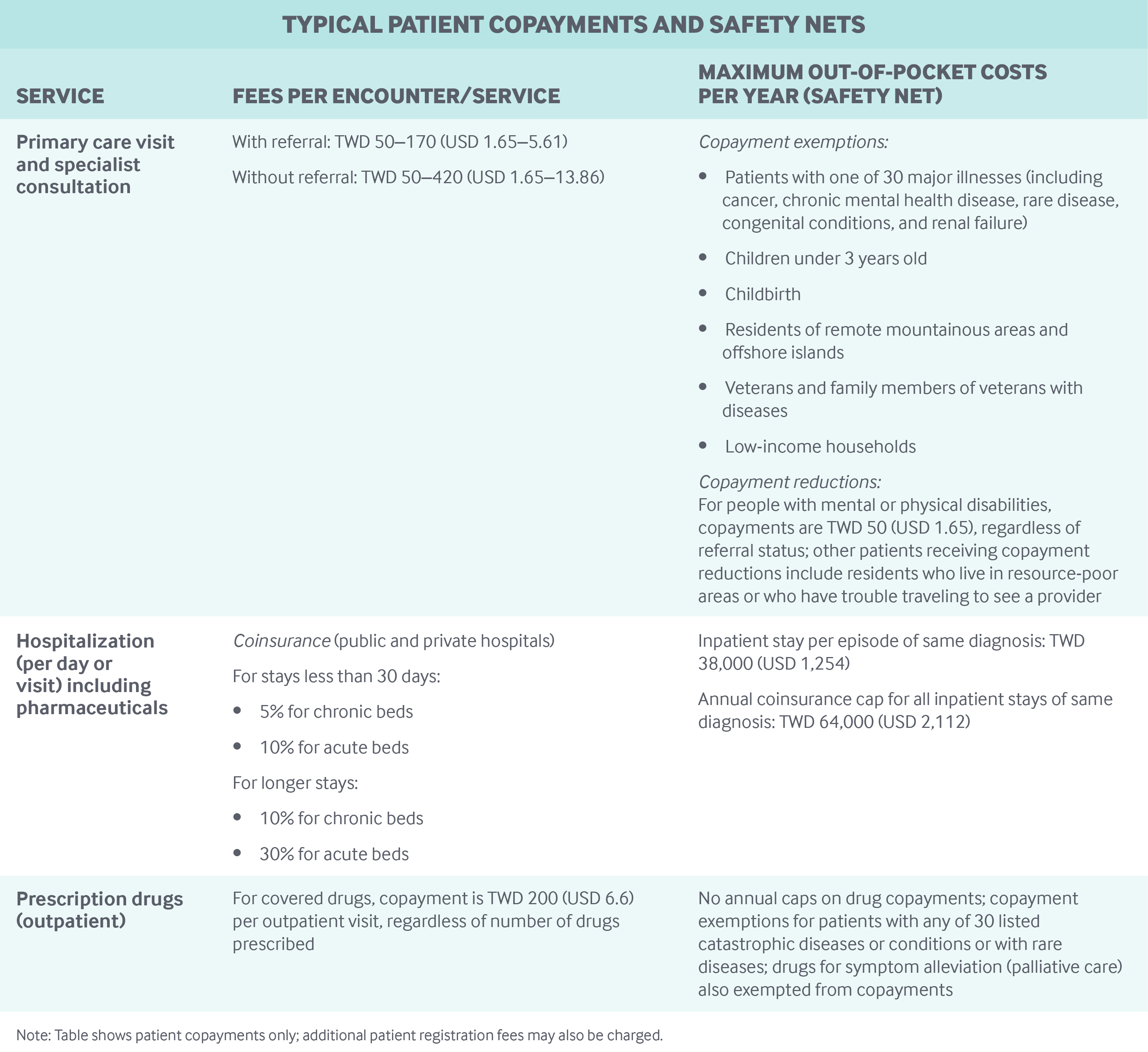
Cost-sharing and out-of-pocket spending: The NHIA mandates copayments for physician visits and prescription drugs, as well as coinsurance for inpatient care, subject to limits and exemptions. There are no annual or quarterly deductibles that must be met.
Copayments for outpatient specialist care range from TWD 50 (USD 1.65) to TWD 170 (USD 5.61) when the patient has a referral from a physician, and TWD 50 to TWD 420 (USD 13.86) without a referral.7,8
Copayments for outpatient prescription drugs covered under NHI are capped at TWD 200 (USD 6. 6) per outpatient visit, regardless of how many drugs are prescribed during that visit. There is no annual cap on drug copayments.
Coinsurance for inpatient care varies by length of stay and type of bed (acute or chronic). For example, the coinsurance rate for an inpatient stay of less than 30 days is 5 percent for chronic beds, and 10 percent for acute beds.9 In 2018, the cap on coinsurance per episode of stay was TWD 38,000 (USD 1,254). For any additional inpatient stays for the same illness or condition, the same cap of TWD 38,000 per stay applies, up to an annual ceiling of TWD 64,000 (USD 2,112) for that particular illness or condition.
Under NHI, all preventive services are free, such as prenatal care, well-baby checkups, Pap smears, breast cancer screenings, adult health checkups, and immunizations. However, clinics and hospitals that deliver such services charge patients a small registration fee.10
In 2016, out-of-pocket health care spending, as officially reported, accounted for 34 percent of total national health expenditures.11 However, in its definition of out-of-pocket spending, Taiwan includes items not counted by the Organisation for Economic Co-operation and Development (OECD), such as infant formula, baby diapers, dietary supplements, health foods, Chinese herbal medicine, private hospital rooms, cosmetic surgery, and high-tech surgical procedures.
According to a former NHIA director-general, out-of-pocket spending associated with necessary health care, including medical care, dental care, and prescription drugs, amounted to 12.1 percent of Taiwan’s national health expenditures in 2012, a figure more in line with the OECD norm.12
Safety nets: In addition to the copayment and coinsurance caps outlined above, the government provides full (100%) premium subsidies for low-income households (1.26% percent of the population in 2018), military personnel, veterans and their dependents, and convicts. The last three groups accounted for 0.48 percent of the population in 2018.
In addition, the government funds varying premium subsidies to other population groups:
- Civil servants, volunteer servicemen, holders of public office, dependents of veterans, and members of farmer, fisherman, and irrigation associations receive premium subsidies of 70 percent.
- Union members, foreign crew members, and nonworking or retired individuals receive premium subsidies of 40 percent.
- Private school teachers get a 35 percent premium subsidy.
- Other employees of public or privately owned enterprises and organizations receive a 10 percent premium subsidy.13
In cases where the insured have lapsed in paying their NHI premiums, full access to care is guaranteed under 2016 government regulations.14
Exemptions from outpatient copayments also apply to certain conditions and population groups, including the following:
- Childbirth
- Thirty specified catastrophic diseases and conditions, including cancer
- Residents of remote and mountainous areas and offshore islands
- Veterans and families of deceased veterans
- Low-income households
- Children under age 3
- Tuberculosis patients.15
Others receive discounts on copayments. For example, outpatient copayments for people with physical or mental disabilities are limited to TWD 50 (USD 1.65), and residents of under-resourced areas receive a 20 percent discount on copayments. In addition, copayments for home care are cut in half (from 10% to 5%) for residents who live in underserved areas or who have difficulty traveling to providers for care.16
Exemptions from drug copayments are given to patients with any of the 30 listed catastrophic diseases or conditions and to patients requiring palliative care or other symptom relief. Finally, the NHIA waives copayments for all drugs necessary to keep people with a list of MoHW-recognized rare diseases alive.
How is the delivery system organized and how are providers paid?
Physician education and workforce: Taiwan's government limits medical school admissions to 1,300 per year. There are both public and private medical schools. In 2018, tuition and fees at public medical schools were approximately TWD 36,170 (USD 1,194) per semester. Private tuition and fees were TWD 72,269 (USD 2,385) per semester.17
Two types of government-sponsored medical education programs help ensure a supply of medical providers in traditionally underserved areas. In the first type, the government may specify what residency-training specialties graduates need to pursue, as well as the location or hospital they need to practice in for two to four years. In the second type, high school graduates from Taiwan's aboriginal communities and offshore islands are admitted, through preferential affirmative action, into either public or private medical schools where they can choose their residency-training specialty but must return to their tribes or offshore islands to practice for six to seven years after graduation.
Physician care: Approximately 40 percent of Taiwan’s physicians practice in their own private clinics. The rest work in hospitals as employees. Eighty percent to 90 percent of clinics are solo practices; the remainder are group practices, which may include multiple specialties.18 In recent years, there has been a trend toward multispecialty group practices.
There is no gatekeeping system in Taiwan. Patients can choose to see any doctor at any time (family medicine or specialist), with no requirement to register with a primary care physician.
When doctors deem it necessary or expedient to refer patients to a higher level of care or another provider (usually a regional hospital or medical center), the patient will pay a lower copayment for that visit. This referral policy is intended to encourage patients with minor illnesses to seek care at local clinics, reducing waste and overcrowding at large hospitals and medical centers and ensuring that patients who truly need tertiary services can access them.
Physicians in Taiwan fall into six specialties: internal medicine, surgery, pediatrics, obstetrics/gynecology, emergency medicine, and “other.” All physicians who practice in clinics are considered primary care doctors in Taiwan. However, only about 5 percent of all clinic doctors have received formal training in primary care.19
Nearly all private clinics (98%) contract with the NHIA to deliver services. Physicians are paid predominantly on a fee-for-service basis, according to national uniform fee schedules set by the NHIA with input from industry stakeholders. A primary care global budget is divided among and managed by the six NHIA regional offices. To maximize revenue, the clinics within each region compete fiercely for patients.
To date, clinic physicians’ financial incentives to change their behavior are relatively limited. On average, less than 1 percent of physician income is derived from capitation or pay-for-performance programs.20 (See “What are the major strategies to ensure quality of care?” below for more on pay-for-performance.)
Other sources of physician income are patient registration fees, services and goods not covered by NHI, and copayments and coinsurance. Physicians, including both family doctors and specialists in private practice, receive the same fees. Fees for psychiatry and emergency medicine are higher.21
Billing above the fee schedule is not permitted, except for a limited number of medical devices. In 2018, these devices included drug-eluting and bioactive coronary stents, ceramic hip joints, and intraocular lens implants.
Hospital-based physicians in all specialties, in both private and public facilities, also see patients on an outpatient basis. As hospital employees, they are paid a salary and bonuses pegged to productivity, such as volume of services delivered or papers published.
There is no specific fee schedule for ancillary medical professionals; most are paid a monthly salary plus a seasonal or annual bonus.22
Administrative mechanisms for direct patient payments to providers: Patients pay copayments at the point of service for physician visits, and pay coinsurance upon hospital discharge. In addition to copayments and coinsurance, clinics and hospitals charge nominal patient registration fees.
After-hours care: There are no formal after-hours care provisions. Although the hospital association and the NHIA have an agreement to provide telephone consultations after hours, the future of the arrangement is uncertain, as physician associations mandate that doctors must rest on weekends.23
Lack of widespread after-hours care is not viewed as a serious problem in Taiwan. Many physician clinics are open until 9:00 p.m. during the week and on Saturdays. Outside these hours, patients may visit one of Taiwan’s more than 400 hospital emergency departments, where access is generally considered convenient and affordable.24 In recent years, however, emergency departments have experienced increasing traffic.
Between 10:00 p.m. and 6:00 a.m., fees for emergency room visits are 50 percent higher than fees charged during the daytime; fees for weekend and holiday visits are 20 percent higher.25
Hospitals: Taiwan has both public and private hospitals. By law, private hospitals are nonprofit. As of 2016, 67 percent of all beds are private.26
Hospitals in Taiwan derive revenues from a global hospital budget set by the NHIA; this system differs from those of many other countries, in which hospitals receive hospital-specific budgets. The global hospital budget is divided into six regional budgets, each administered by one of six NHIA regional offices. Under this arrangement, competition for revenues is intense among hospitals within each region. Hospital business strategies include mergers, to expand market share, and direct-to-consumer advertising.
Hospitals are paid fee-for-service according to uniform national fee schedules and diagnosis-related groups (DRGs) set by the NHIA with input from stakeholders. As of 2016, there were 401 DRGs, accounting for 22 percent of all hospital payments. Uptake of DRGs has been slow, owing to provider resistance.
Hospitals also derive revenues from direct payments for non-NHI-covered services and goods, copayments for outpatient services and coinsurance for inpatient services, and registration fees collected at the time of service.
Mental health care: NHI covers mental health services on an outpatient basis (including day care), and on an inpatient basis for both acute and chronic mental health problems. Over the past 15 years, Taiwan has been increasing its mental health bed capacity to alleviate a shortage in the supply of such beds.
All copayments associated with chronic mental health care are waived.27
Long-term care and social supports: As of 2017, 14 percent of Taiwan's population was aged 65 or older. In response to Taiwan's rapidly growing elderly population, the government has implemented a long-term care policy that seeks to integrate medical care, long-term care, prevention, and health maintenance to facilitate aging in place, healthy aging, and active aging.
In October 2016, the government began a trial implementation of its 10-Year Long Term Care Plan 2.0. A new service delivery system is being developed to provide services through a three-tiered, community-based network:
- Level A agencies, or community-based service centers, are responsible for preparing care plans for individuals with cognitive impairments.
- Level B agencies are connected to Level A agencies and are responsible for delivering long-term care services.
- Level C agencies, or neighborhood long-term care stations, are connected to Level B agencies and are responsible for providing preventive and disability delay services.
Communities may elect to implement either an A-B-C network model or a B-C network model of delivery.
Both public and private hospitals and medical centers participate in the three-tier long-term care service delivery.
Services covered include home care, day care, transportation, meals, purchase and rental of equipment, home accident-proofing, home nursing care, home and community rehabilitation services, respite care, caregiver support services, and training to prevent or delay the onset of disabilities (e.g., swallowing and muscle strength training).
Enrollment in long-term care coverage is mandatory starting at birth. Financing currently relies on three sources: government, employers, and out-of-pocket payments by users of services. For low-income families, the government subsidizes 100 percent of long-term care costs.
As of June 2019, long-term care remains a work in progress in Taiwan.
What are the major strategies to ensure quality of care?
Major NHIA strategies to ensure quality of care fall into three broad categories:
Payment incentives. A number of programs aim to improve access and quality, such as the pay-for-performance schemes. Since 2001, pay-for-performance programs have been implemented for 12 diseases and conditions including cervical cancer, tuberculosis, diabetes, asthma, schizophrenia, early-stage chronic kidney disease, and maternity care. Care teams consisting of nurses, dieticians, and other nonphysician clinicians provide integrated and coordinated care to improve quality and outcomes.
The program is reaching many of Taiwan’s people. For instance, as of 2017, 68 percent of schizophrenia patients are cared for under the pay-for-performance plan.28
The annual budgeting process is also incentivized. Taiwan has five sectoral global budgets, for dentistry, Chinese medicine, primary care clinics, hospitals, and dialysis. Each July, the NHI Committee meets with scholars and experts to review and grade the performance of each sectoral global budget in terms of service delivery, quality, public satisfaction, appropriate use of resources, and other criteria. There are five grades: “exceptional,” “excellent,” “good,” “fair,” and “bad.” (A “bad” grade has never been assigned.)
The annual increase for each sectoral global budget is based on the grade received: a 0.5 percent increase for “exceptional,” 0.3 percent for “excellent,” and so on.
Claims management and reviews: Taiwan has a fully automated claims review system to ensure that claims meet specific medical appropriateness criteria. In addition, randomly selected claims are peer-reviewed for consistency in billing and for the clinical appropriateness of treatments.
Information-sharing and transparency: Since 2005, the NHIA has publicly reported provider performance data on specific quality and cost metrics, including registration fees charged, health care services provided, and the quality of services (including hospital-acquired infection rates) to facilitate patient decision-making on where to seek care.
The NHIA has developed several hundred quality indicators, some of which are used in pay-for-performance programs, some for calculating global budgets, and others for public transparency efforts and claims review.29 Many of these metrics serve the dual purpose of improving quality and reducing costs.
Other important national programs for quality assurance and improvement include:
- The Post-Acute Care Pilot Project for stroke patients
- The Integrated Post-Acute Care program for burn patients
- The Artificial Joints Registry System, which was launched in 2016 to improve patient safety and quality of care and reduce mortality from unsafe artificial joints.
What is being done to reduce disparities?
More than 3 million economically disadvantaged Taiwanese (12.8% of the population) have full access to NHI services, owing to the NHIA’s various financial and access-assistance measures, including premium subsidies and copayment and coinsurance reductions or exemptions (see “Safety nets” in table above). The NHIA also makes interest-free loans and installment plans available to those who cannot pay their premiums on time because they are temporarily unemployed or between jobs. In recent years, the government has lowered the income threshold to allow more people to become eligible for these premium subsidies.
What is being done to promote delivery system integration and care coordination?
In general, financial incentives that encourage physicians to provide coordinated care are relatively limited.30 In addition, programs integrating health and social care services for vulnerable populations are currently a work in progress. Three departments within the MoHW currently provide social care services, but full integration with health care services has not yet occurred. Funding for social care services comes from budget allocations to municipal governments.
However, improving delivery system integration and care coordination has been on the NHIA’s agenda for many years. Efforts to date include:
The Integrated Delivery System. Taiwanese living in remote and mountainous areas and on offshore islands (approximately 400,000 people, or 1.7% of the population) can access medical services through the Integrated Delivery System, a government program that began in 1999. The program provides access to outpatient care (including overnight and on holidays), 24-hour emergency care, and specialty care through integrated village clinics, local hospitals, and mobile health services. Telemedicine and helicopter services are used to provide needed care to patients on remote offshore islands, for example, and to bring pregnant women to hospitals for delivery.
As part of the program, providers receive bonuses for serving these remote patients.
The Family Doctor Integrated Care Program. Since 2003, the NHIA has been promoting this community-based program. Community networks, made up of five or more primary care physicians and one community hospital, provide patient-centered primary care, including disease management, patient health education, and preventive care. Telephone consultations with family doctors are also available 24 hours a day for people enrolled in the program.
In 2017, the Family Doctor Integrated Care Program was strengthened with an increased emphasis on service capacity and quality improvement in community-based medical networks.
As of June 2017, 4,063 primary care clinics and 183 hospitals have joined to form 526 primary care networks, covering 4.1 million residents, or 17.4 percent of NHI enrollees in Taiwan.31 Primary care networks are paid small fees for registering patients in their network.
The Hospital Patient-Centered Integrated Care Program. This initiative is aimed at outpatients aged 65 and older with two or more chronic conditions.
What is the status of electronic health records?
Everyone in Taiwan carries an electronic NHI card bearing a unique personal identifier to access care. The card encodes personal information, insurance data, notes from recent medical visits, diagnoses, drug prescriptions, drug allergies, major illnesses, organ donation consent, palliative care directives, and public health records (including immunizations).
The NHI PharmaCloud is a cloud-based, patient-centered drug information system that the NHIA introduced in 2013. PharmaCloud takes advantage of the vast database the NHIA has created to enable doctors and pharmacists to access a patient’s medication history from the past three months. PharmaCloud also gives prescribers clinical recommendations and safe-use information to prevent adverse drug reactions and reduce unnecessary prescriptions.
My Health Bank, introduced in 2014, is another cloud-based innovation that provides comprehensive health and medical records from the previous three years for any insured person on request. Records can be updated at any time. In addition to increasing the transparency of important personal health information, the initiative is intended to assist patients in managing their own health. A personal e-health record book contains the patient's complete medical history from the past year, which can be downloaded from the Web for the patient's own use.
In 2015, the NHIA developed the NHI MediCloud system, which incorporates patient data in the PharmaCloud system and in 11 additional records systems; the data includes Chinese medicine prescription use, examination and test results, surgeries, dental care and oral surgery, drug allergies, and hospital discharge summaries.32
All hospitals and clinics use electronic patient medical records. However, owing to a lack of infrastructure investment, NHI still has no systemwide interoperability, and the electronic exchange of patient medical records among hospitals is limited.33
How are costs contained?
The global NHI budget system is, by far, Taiwan’s most powerful cost-containment tool. After global budgets were introduced, national health expenditures grew by 3.87 percent a year on average between 2004 and 2015. Prior to that period, annual growth rates ranged from 6 percent to 9 percent.
Other cost-containment measures include DRG payments for hospitals and annual drug price adjustments.
Drug expenditures account for 25 percent of total NHI expenditures, higher than the OECD average of 16.2 percent.34 Prices for pharmaceuticals are set by the NHIA with input from stakeholders. The NHIA’s pharmaceutical benefit management initiative considers both clinical effectiveness and cost-effectiveness in coverage decisions. Prices for breakthrough drugs that are under patent protection are set through reference pricing, in accordance with the median price in 10 leading developed countries: the U.S., the U.K., Australia, Belgium, Canada, Germany, France, Japan, Sweden, and Switzerland.35
To control total drug expenditures as a percentage of total NHI expenditures, the NHIA implemented an annual price adjustment mechanism in 2013. When actual drug expenditures (billings) exceed target expenditures in any given year, the automatic price adjustment mechanism kicks in, and prices are revised so that total expenditures do not exceed the predetermined target.36
As noted earlier, the NHIA’s automated claims review checks for the overall appropriateness of claims; in addition, the IT system randomly selects a small percentage of claims for individual professional review by clinical experts. Both measures are aimed at monitoring cost and quality.
Patient cost-sharing has never been a key cost-containment strategy in Taiwan. Overall, government provisions aimed at safeguarding access to care have rendered patient cost-sharing a largely insignificant factor in cost containment.
Political considerations have made eliminating low-value care difficult.37
What major innovations and reforms have recently been introduced?
Since June 2016, the NHIA has stepped up efforts aimed at strengthening primary care through delivery system integration and the establishment of a referral system. The six components of this new strategy38 are:
- Enhancing the capacity of primary care
- Incentivizing the public to use the referral system through adjustments to the copayment system
- Raising payments to hospitals for critical care to incentivize hospitals to reduce services related to treating minor illnesses
- Strengthening cooperation between hospitals and clinics to provide continuous care
- Strengthening the public's capabilities in self-care
- Strengthening the governance of hospitals.