By Isabelle Sturny, Swiss Health Observatory
Switzerland’s universal health care system is highly decentralized, with the cantons, or states, playing a key role in its operation. The system is funded through enrollee premiums, taxes (mostly cantonal), social insurance contributions, and out-of-pocket payments. Residents are required to purchase insurance from private nonprofit insurers. Adults also pay yearly deductibles, in addition to coinsurance (with an annual cap) for all services. Coverage includes most physician visits, hospital care, pharmaceuticals, devices, home care, medical services in long-term care, and physiotherapy. Supplemental private insurance can be purchased for services not covered by mandatory health insurance, to secure greater choice of physicians, and to obtain better hospital accommodations.
Sections
How does universal health coverage work?
Historically, health insurance in Switzerland had been provided by many small private insurers. After several attempts to introduce a system of universal coverage, the federal government adopted the Health Insurance Law in 1994, based on a private insurance model. The law’s objectives were to:
- strengthen equality by introducing universal coverage and subsidies for low-income households
- expand the benefit basket and ensure high standards of health services
- contain the growing costs of the health system.1
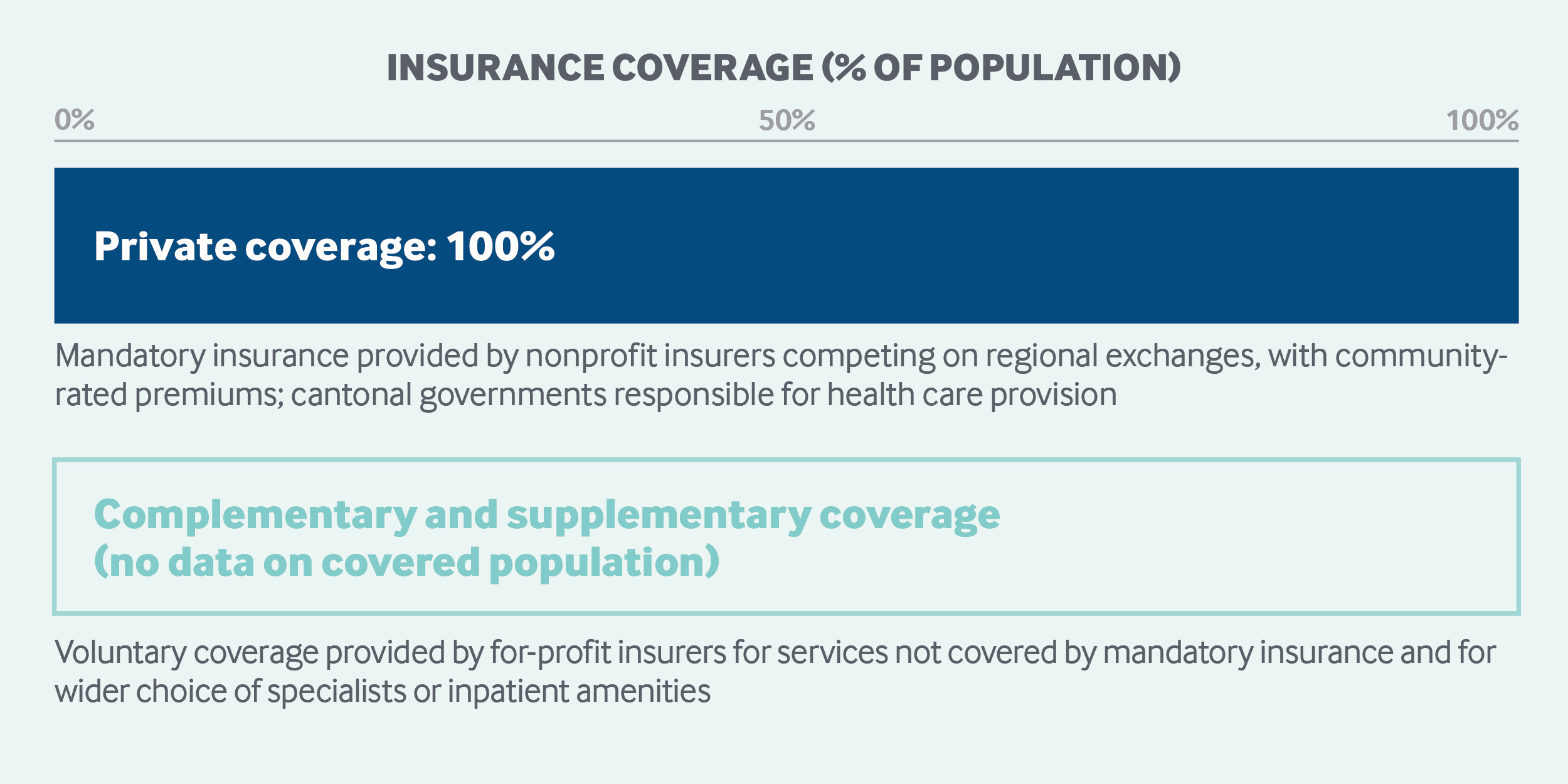
Since going into effect in 1996, health insurance coverage is close to 100 percent. Citizens are legally required to purchase insurance, and the cantons ensure compliance. Insurance policies typically apply to individuals, and separate coverage must be purchased for dependents. New residents must purchase a policy within three months of arriving in Switzerland, and coverage applies retroactively to the arrival date. Temporary nonresident visitors pay for care themselves and claim expenses from any insurance coverage they hold in their home countries. The absence of mandatory health insurance for undocumented immigrants remains an unsolved problem.
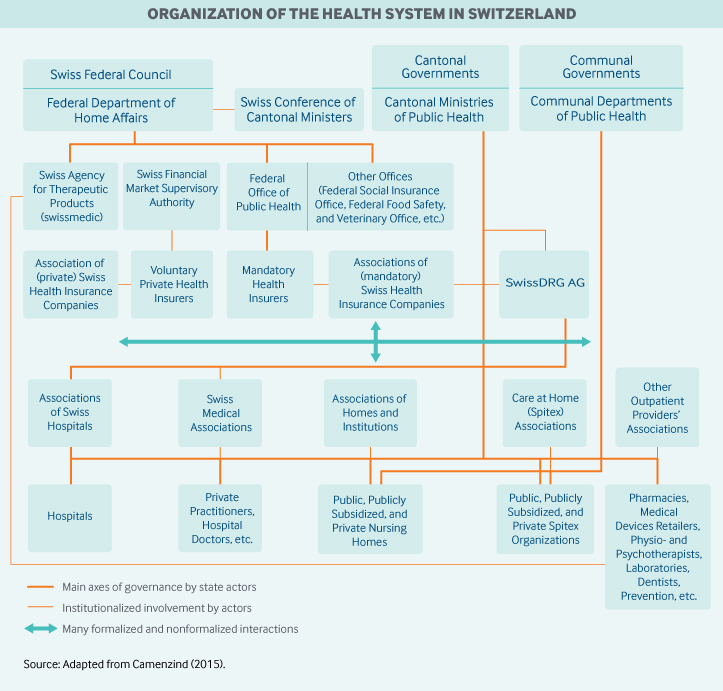
Role of government: Duties and responsibilities in the Swiss health care system are divided among the federal, cantonal, and municipal governments. Each of the 26 cantons has its own constitution and is responsible for licensing providers, coordinating hospital services, promoting health through disease prevention, and subsidizing institutions and individual premiums. The federal government regulates system financing, ensures the quality and safety of pharmaceuticals and medical devices, oversees public health initiatives, and promotes research and training. The municipalities are responsible mainly for organizing and providing long-term care (nursing home care and home care services) and other social support services for vulnerable groups.
Since health care is largely decentralized, the key entities for health system governance exist mainly at the cantonal level. Each canton has its own elected minister of public health; a coordinating political body, the Swiss Conference of Cantonal Health Ministers, plays an important role.
Other important health-related agencies include the following:
- The Federal Office of Public Health, which is the main national player, supervises the legal application of mandatory health insurance, authorizes statutory insurance premiums, governs statutory coverage (including health technology assessment), and determines the prices of pharmaceuticals. The agency is also responsible for national health strategies, including health promotion, disease prevention, and health equity.
- The Swiss Federal Department of Home Affairs formally defines the mandatory health insurance benefit basket by evaluating whether services are appropriate and cost-effective. It is supported in this task by the Federal Office of Public Health and by Swissmedic, the agency that authorizes and supervises therapeutic products.
- The nonprofit corporation SwissDRG AG is responsible for defining, developing, and adapting the national system of relative cost weights per case used for determining provider payment for inpatient services.
- Health Promotion Switzerland, a nonprofit organization, is legally charged with health promotion programs and provides public information on health.
- The Association of Swiss Patients and a national ombudsman for health insurance engage in patient advocacy.
Role of public health insurance: In 2016, total health expenditures represented 12.2 percent of Switzerland’s GDP, or CHF 80.7 billion (USD 66.7).2,3 Publicly financed health care accounts for 62.8 percent of health spending, or 7.7 percent of GDP. The public health insurance system has three streams of funding:
- Mandatory health insurance premiums accounted for 35.6 percent of total health spending in 2016.
- General taxes financed 17.3 percent of total health expenditures in 2016, with cantonal taxes accounting for 15.0 percent, municipal taxes for 1.8 percent, and federal taxes for 0.4 percent.
- Contributions to other social insurance schemes, including military, old-age, and disability insurance, made up 10.0 percent of spending in 2016.
Mandatory health insurance is offered by competing nonprofit insurers on cantonal exchanges. It is not sponsored by employers. The insurers are supervised by the Federal Office of Public Health.
The 56 insurers on the exchanges provide policies for three distinct age groups — children through age 18, young adults 19 to 25, and adults 26 and above — each at six different deductible levels. In addition to the standard coverage model (basic coverage with free choice of doctor), there are various alternatives that restrict provider choice: health maintenance organizations (HMOs); family doctor models, which require an initial consultation with the family physician (gatekeeper) in the event of illness; and call-center models, under which patients call a consultation hotline prior to seeing a doctor. In 2016, 65.7 percent of those insured chose an alternative insurance plan.4 Some health plans also offer accident coverage.
In 2018, the average annual premium across Switzerland was CHF 5,584 (USD 4,615). However, there can be significant variation in premiums among insurers and insurance plans. In 2018, the average annual cantonal premium ranged from CHF 4,248 (USD 3,511) to CHF 7,102 (USD 5,869) for adults with a standard insurance model, accident coverage, and the minimum deductible of CHF 300 (USD 248).5
Individuals pay premiums through the insurer of their choosing. Then funds are redistributed among insurers by a central fund, in accordance with a risk-equalization scheme that is adjusted for canton, age, gender, and major expenditures in the previous year, such as hospital or nursing home stays and pharmaceutical costs.
Role of private health insurance: Voluntary health insurance accounted for 6.7 percent of total expenditures in 2016. No data are available on the number of people covered by these plans. Residents use voluntary health coverage to pay for services not covered by mandatory health insurance and to ensure free choice of hospitals or doctors and preferred hospital accommodation.
Voluntary health insurance is regulated by the Swiss Financial Market Supervisory Authority. Insurers can vary benefit baskets and premiums and can refuse applicants based on medical history. Service prices are usually negotiated directly between insurers and providers.
Unlike statutory insurers, voluntary insurers are for-profit; an insurer will often have a nonprofit branch offering mandatory health insurance and a for-profit branch offering voluntary insurance. It is illegal for voluntary insurers to base voluntary insurance subscription decisions on health information obtained via basic health coverage, but this rule is not easily enforced. Employers do not offer voluntary insurance.
Services covered:
Mandatory health insurance covers the following:
- hospital inpatient services
- most general practitioner (GP) and specialist services
- an extensive list of pharmaceuticals and medical devices
- home care services (called Spitex)
- physiotherapy (if prescribed)
- some preventive measures, including selected vaccinations, selected general health examinations, and screenings for high-risk patients
- maternity care, including prenatal checkups, birth, postpartum care, and breastfeeding advice
- outpatient care for mental illness, if provided or delegated by physicians
- medically necessary long-term care
- hospice care if there is an underlying disease.
Durable medical equipment, such as wheelchairs, is not covered, and hearing aids are financed only if not covered by old-age and disability insurance. Dental care is largely excluded for adults, as are glasses and contact lenses for adults (unless medically necessary); however, these services and supplies are covered for children up to age 18.
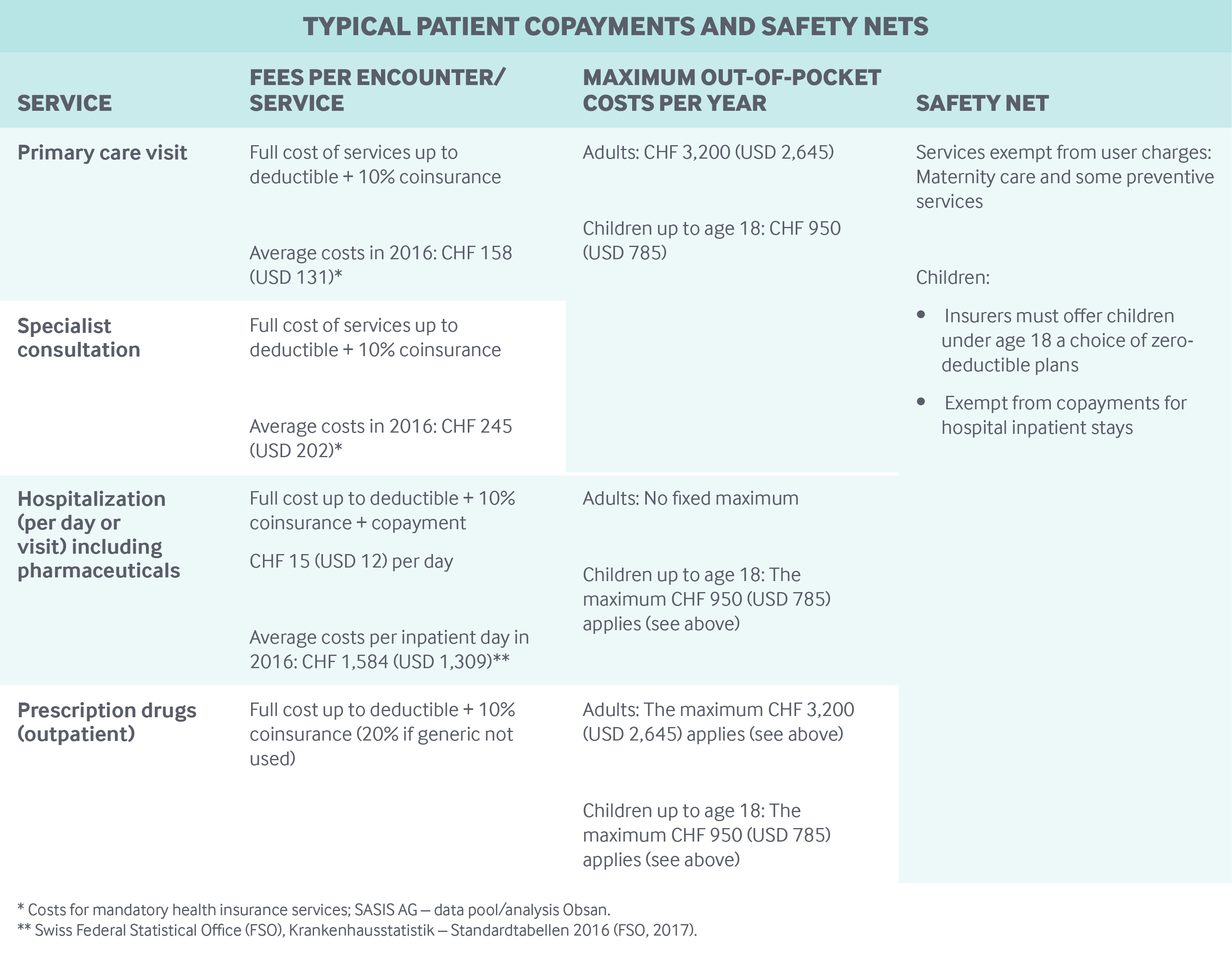
Cost-sharing and out-of-pocket spending: Under mandatory health insurance, insurers are required to offer a minimum annual deductible of CHF 300 (USD 248) for adults and a zero deductible for children through the age of 18. Insured persons may opt for a higher deductible of up to CHF 2,500 (USD 2,066) for adults and CHF 600 (USD 496) for children, with a lower premium.
In 2016, about 54 percent of all insured persons opted for an insurance model with the minimum deductible of CHF 300/0 (USD 248/0), and about 46 percent chose a model with a higher deductible and a lower premium.6
In addition to deductibles, insured persons pay 10 percent coinsurance for all services (except for maternity care and some preventive services), with a cap of CHF 700 (USD 579) per year for adults and CHF 350 (USD 289) for children through age 18. For brand-name drugs that have a generic alternative, 20 percent coinsurance is charged instead of 10 percent. For hospital stays, there is an additional CHF 15 (USD 12) copayment per inpatient day.
Cost-sharing in Switzerland’s mandatory health insurance program accounted for 5.3 percent of total health expenditures in 2016.7
Safety nets: Maternity care and some preventive services (mammograms and colorectal cancer screenings) are fully covered and are therefore exempt from deductibles, coinsurance, and copayments. Children or young adults in school (through age 25) are exempt from copayments for inpatient care.
The federal government and the cantons provide income-based subsidies to some individuals or households to cover mandatory health insurance premiums; income thresholds vary widely by canton.8 Overall, 27.3 percent of residents in 2016 benefited from individual premium subsidies.9 Municipalities or cantons cover mandatory health insurance expenses for social assistance beneficiaries and recipients of supplementary old-age and disability benefits. There is also a maximum user charge for prescription drugs and primary and specialty care — for adults, CHF 3,200 (USD 2,645. There is no maximum user charge for hospital care provided to adults (see table).
How is the delivery system organized and how are providers paid?
Physician education and workforce: Medical training takes place in public universities in a six-year program. After receiving the federal medical diploma, graduates enter the specialist training phase. The title of “specialist” is one of the conditions for practicing medicine in an independent medical practice.
Although increasing the national capacity for the training of health workers is a high priority of the Health2020 strategy,10 entry restrictions may apply at certain universities. Training requirements are determined at the federal level. Tuition fees vary by the university chosen and range between CHF 1,000 (USD 826) and CHF 1,700 (USD 1,405) for Swiss students. Some cantons offer scholarships to help cover tuition fees.
The responsibility for ensuring an adequate supply of medical providers lies with the cantons.
Primary care: Registering with a GP is not required, and most people generally have free choice among self-employed, private GPs, except those enrolled in managed-care plans. In 2017, 42.9 percent of doctors in the outpatient sector were classified as GPs (including pediatricians). While 53.7 percent of physicians (GPs and specialists) were in solo practice, the remainder were in practices with an average of 4.2 physicians.11 The median number of patients per GP practice was 1,779 in 2015.12
Primary (and specialist) care tends to be physician-centered, with nurses and other health professionals playing a relatively small role. Regional medical networks with shared resources and coordination between all stakeholders are becoming more common.
There are no specific financial incentives for GPs to take care of chronically ill patients, and no concrete reform efforts are under way to engage GPs in bundled payments for patients with a chronic illness, such as diabetes. Apart from some managed-care plans in which physician groups are paid through capitation, most GPs are paid according to a national fee-for-service scale, called TARMED, which was introduced in 2004. TARMED fees are negotiated annually between the health insurers’ associations and cantonal provider associations or may be set by cantonal government if the parties cannot agree. Billing above the fee schedule is not permitted.
The median income of primary care doctors was CHF 236,885 (USD 195,772) for independent physicians and CHF 155,752 (USD 128,721) for employed physicians in 2014; these were lower than the average median income of all specialists.13
Outpatient specialist care: In the outpatient sector, 57.1 percent of doctors in private practices were classified as specialists in 2017; they are mostly self-employed.14 Residents have free access (without referral) to specialists unless enrolled in a managed-care plan with gatekeeping.
Like GPs, specialists are paid fee for service in accordance with TARMED and cannot bill above the fee schedule. There are also no incentive payments for specialists.
Specialist practices tend to be concentrated in urban areas and within proximity of acute-care hospitals. The Swiss system allows specialists to see patients with private insurance as well as mandatory insurance.
Administrative mechanisms for direct patient payments to providers: Mandatory health insurance allows different methods of payment: Providers can invoice the patient, who makes the initial payment and claims reimbursement from the insurer retrospectively. Alternatively, providers can bill the insurer directly for the entire sum. The insurer then bills the patient for any coinsurance or copayments owed.
After-hours care: The cantons are responsible for after-hours care. They delegate the services (with fees set by TARMED) to cantonal doctors’ associations, which organize urgent-care networks in collaboration with their affiliated doctors. Swiss physicians are not statutorily required to provide after-hours care through these networks.
The networks can include ambulance and rescue services, hospital emergency services, walk-in clinics (hospital-based or stand-alone), and telephone advice lines that are run or contracted by insurers. These services are mostly available 24/7. Staffing patterns and the use of nurse triage in these networks vary between localities.
There are no formal processes for the exchange of information between these services and GPs’ offices, as people are not required to register.
Hospitals: In 2016, there were 283 hospitals (102 general and 181 specialty hospitals), with a total of 38,058 beds.15 Hospitals are publicly or privately owned. Hospital care represented one-third (35.3%) of total health expenditures in 2016.
Hospitals receive at least 55 percent of their funding from cantons.16,17 The rest is covered by mandatory health insurance and by coinsurance and copayments from patients. Services covered by mandatory health insurance are billed through the national diagnosis-related group (DRG) payment system. There are no pay-for-performance initiatives.
The cantons are responsible for hospital planning and are legally bound to coordinate plans with other cantons. Since 2012, patients have been free to obtain care in any canton. Remuneration mechanisms depend on insurance contracts; consequently, fee-for-service for inpatient services not covered under mandatory health insurance is still possible.
Hospital-based physicians are normally paid a salary, and public-hospital physicians can receive extra payments for seeing privately insured patients.
Mental health care: Care for mental illnesses is covered by mandatory health insurance if provided by certified physicians, including psychiatrists. The services of nonphysician professionals, such as psychotherapy provided by psychologists, are covered only if prescribed by a qualified medical doctor and provided in his or her practice.
Psychiatric hospitals normally provide a full range of services, such as psychiatric diagnostics and treatment, psychotherapy, pharmaceutical treatment, and forensic services. Clinics are most commonly specialized in specific conditions.
There is also a wide range of socio-psychiatric facilities and day care institutions that are run and funded mainly by the cantons. Often, the socio-psychiatric facilities and day care institutions offer the same services as the clinics, but normally treat patients with less-acute symptoms.
Psychiatric care is not systematically integrated into primary care. Some GPs provide mental health services.
Long-term care and social supports: Some long-term care services are covered under mandatory health insurance. Inpatient care is provided in nursing homes and institutions for disabled and chronically ill persons. Patients receive outpatient home care through specialized organizations.
Coverage for palliative care provided in hospitals, in nursing homes, in hospices, or at home is similar to coverage for acute services in these provider settings. Hospice care is covered as long as there is an underlying disease.
There is no provision of individual or personal budgets for patients to organize their own services, nor is there financial support at the national level for informal hired help or family caregivers.
For services in nursing homes and institutions for disabled and chronically ill persons, mandatory health insurance pays a contribution to cover care-related, medically necessary costs; the patient pays at most 20 percent of care-related costs, and the remaining care-related costs are financed by the canton or the municipality.
Long-term inpatient care costs represented 16.1 percent of total health expenditures in 2016. Thirty-six percent of these costs were paid by private households, 24 percent by government subsidies, 22 percent by old-age and disability benefits, and 18 percent by mandatory health insurance and other social insurances.
Of the 1,570 nursing homes in operation in 2016, 27.5 percent were state-operated and state-funded, 27.5 percent were privately operated with public subsidies, and 45 percent were exclusively private.18 In 2016, 56 of every 1,000 people over age 65 were in nursing homes.
Home care providers (Spitex) represented 1.7 percent of total health expenditures in 2016. More than half (57.8%) of these costs are financed by mandatory health insurance and the other social insurances. The insurers limit their contributions to medically necessary health care at home. Government subsidies made up roughly one-third of total Spitex spending (29.4%). The rest (12.8%), devoted mainly to support and household services, was typically paid out-of-pocket or covered by old-age and disability benefits, by voluntary health insurance, or by other private funds.19 In 2016, 31 percent of Spitex providers were subsidized nonprofit organizations, 20 percent were nonsubsidized for-profit companies, and 49 percent were individual health care workers.20
What are the major strategies to ensure quality of care?
Providers must be licensed to practice medicine and are required to meet educational and regulatory standards; continuing medical education for doctors is compulsory. The Swiss Institute for Continuing Medical Education is responsible for accreditation.
Professional self-regulation has been the traditional approach to quality improvement. This is increasingly being challenged. Local quality initiatives, often at the provider level, include the development of clinical pathways, medical peer groups, and consensus guidelines. However, there are no explicit financial incentives for providers to meet quality targets.
Increasing the quality of care is a priority of the federal Health2020 initiative. The strategy includes the implementation of a national network for quality and national quality programs in fields like medication safety and hospital infections.21
In 2008, the Swiss Inpatient Quality Indicators were introduced to monitor and evaluate the quality of care provided by acute-care hospitals. In addition, the National Association for Quality Improvement in Hospitals and Clinics publishes quality indicators for hospital inpatient care based on registries or patient satisfaction surveys. Some registries are the result of private initiatives; others, such as the cantonal cancer registries, are organized by the cantons. There are currently no publicly available data regarding physician or nursing home performance.
Since the association Smarter Medicine – Choosing Wisely Switzerland was founded in 2017, several medical societies have published top-five lists of treatments that are unnecessary and should therefore no longer be performed or reimbursed.
What is being done to reduce disparities?
The Swiss Federal Council’s national Health2020 strategy explicitly calls for improving health opportunities for the most vulnerable population groups, such as children, people with low incomes or poor educational backgrounds, the elderly, and immigrants.22 The aim is to facilitate easier access to necessary health care services.
Toward this purpose, the Federal Office of Public Health supports various initiatives to strengthen the health literacy of disadvantaged people and the competence of health professionals. From 2012 to 2017, these efforts focused mainly on the migrant population; today, the programs are broader in scope.
Starting in 2018, the National Strategy for the Prevention of Non-communicable Diseases and the National Strategy on Addiction and Mental Health have focused on health equity.23 In addition, health and health access variations (by region and socioeconomic characteristics) are measured and reported publicly by the Swiss Health Survey every five years.24
What is being done to promote delivery system integration and care coordination?
Care coordination is an issue, particularly in light of a projected future shortage of health professionals and the need to improve efficiency to increase capacity. The national Health2020 strategy states that integrated health care models need to be supported, especially for patient groups that use many different and complex health care services.
To improve coordination, networks of experts are addressing important challenges such as palliative care, dementia, noncommunicable diseases, and mental health. They are designing pilot projects aimed at encouraging different types of health professionals to work together. In addition, the Forum for Managed Care awards a prize every year to promote innovative cross-sector networking projects in the Swiss health care sector.
The Federal Office of Public Health is also working on improving the framework for coordinated care, mainly in the areas of finance, education, and electronic health records (EHRs). The National Health Report 2015 discusses a growing number of case management programs for chronically ill patients, but pooled funding streams do not yet exist.25
What is the status of electronic health records?
In June 2015, a law addressing a national EHR was adopted; it came into effect in 2017. By spring 2020, an EHR with unique identifiers will be rolled out in all regions and should increase care coordination, quality of treatment, patient safety, and efficiency in the health care system. EHealth Suisse, a joint initiative of the federal and cantonal governments, is coordinating the introduction of the EHR.
The program is voluntary; insured persons are free to opt in to the EHR and to decide who is allowed to have access to specific details of their treatment-related information. The records are being stored in decentralized form.
Providers will have to take part in certified communities (organizational units of health specialists and their institutions) to be able to read the records. While ambulatory-care providers are not obliged to join such communities, hospitals and long-term care institutions are legally bound to join and to offer their services using the EHR.
The uptake of the EHR in primary care is still in its early stages. Forty percent of physicians and outpatient centers handle their medical records exclusively on paper, and there are ongoing discussions about incentives for physicians to adopt new technologies.26 Hospitals are generally more technologically advanced; some have merged their internal clinical systems with external providers. However, the extent of this integration varies greatly among hospitals and among cantons.
How are costs contained?
Switzerland’s health care costs are the second-highest in the world. The Swiss Federal Department of Home Affairs postulated in 2013 that the costs of providing mandatory benefits in the health system could be reduced by up to 20 percent.27 The Health2020 strategy lists possible cost-reducing measures, including:
- further flat-rate remuneration mechanisms, such as capitation
- revision of existing fee schedules to eliminate existing incentives for expensive and unnecessary services
- the concentration of highly specialized medicine for greater efficiency
- improvements in quality of treatment through use of more-experienced provider teams.
In 2012, DRGs were introduced to contain hospital inpatient costs. In addition, as of January 2019, certain hospital treatments must be provided in an outpatient setting in cases where patients will not be put at risk.
Inpatient capacity is subject to cantonal planning to prevent overcapacity. To limit the number of new physicians and to control escalating costs, a temporary ban on setting up new outpatient practices has been in place on and off since 2002 and is in force until 2021. But, given concerns over the supply of primary care physicians, particularly in rural areas, the federal government adopted a constitutional article in 2014 aimed at strengthening primary care.
To control pharmaceutical costs, coverage decisions on all new medicines are subject to an evaluation of their effectiveness and cost. Efforts are being made to reassess the prices of one-third of existing drugs every year. Depending on national market volume, generics must be sold for 20 percent to 50 percent less than the original brand. In addition, consumers pay higher coinsurance for brand-name drugs if generics exist. Pharmacists are reimbursed flat amounts for prescriptions, so they have no financial incentive to dispense more-expensive drugs.
In 2018, the Federal Office of Public Health launched a cost-containment program that places responsibility for reducing expenses on all health care actors. The first package of measures, nine in all, was adopted in 2019 and features improved cost-control and tariff schemes and a reference price system for pharmaceuticals. In 2020, a second package of initiatives is anticipated to increase cost transparency and improve coordinated care.
What major innovations and reforms have recently been introduced?
As discussed throughout this profile, the Health2020 strategy outlines national priorities, objectives, and 36 different measures aimed at:
- improving the quality of life
- promoting equal opportunity and self-responsibility
- ensuring and enhancing the quality of care
- creating more transparency, better governance, and closer coordination.
Recent reforms focus mainly on cost containment (see above).
The author would like to acknowledge Paul Camenzind and David Squires as contributors to earlier versions of this profile.28

